
INCT- Biofabris
Tomography images of patient, 3D model of the skull and made-to-measure prosthesis designed on softwareINCT- BiofabrisA made-to-measure titanium prosthesis transformed the life of a 23-year-old student, Jessica Alves Farias Cussioli. After a serious accident in September 2014, in Araçatuba, São Paulo State, when she fell from a motorcycle and hit her head against a dumpster, Jessica had a deep indentation on the right side of her skull, in an area between her eyes and the top of her head. Eight months later, on May 26, 2015, she became the first patient in Brazil to receive a titanium craniofacial implant, a procedure done at the Hospital das Clínicas of the University of Campinas (HC-Unicamp). The manufacture of the made-to-measure prosthesis by the National Institute of Science and Technology in Biomanufacturing (INCT-Biofabris), headquartered at Unicamp and funded by FAPESP and the National Council for Scientific and Technological Development (CNPq), is part of a long process of multidisciplinary research and development that began in 2009.
In addition to Unicamp, members of Biofabris include such institutions as the University of São Paulo (USP), the Federal University of São Paulo (Unifesp) the University of Rio Grande do Sul (UFRGS), the Nuclear and Energy Research Institute (IPEN) and the Renato Archer Information Technology Center (CTI). “We work on the development of polymers, biopolymers, metal and ceramic materials, intended for various applications,” says Rubens Maciel, a chemical engineer and professor at the School of Chemical Engineering (FEQ) of Unicamp and Biofabris coordinator. Studies on the development of new materials still involve in vitro and in vivo tests to determine whether or not they will harm the patient upon implantation in the future. “Their performance in the body must not be harmful to cells nor harm the body in the implanted area.”
Jessica’s operation lasted more than eight hours and was performed by a medical team consisting of four plastic surgeons and a neurosurgeon. The surgical procedure was the culmination of a collaborative effort involving doctors and researchers over a period of three months. The partnership between the Institute and the HC-Unicamp started shortly after the founding of Biofabris. “After a long conversation with Rubens Maciel and Andre Jardini [a mechanical engineer and researcher at Biofabris Institute], I realized that we could form a scientific partnership,” says Paulo Kharmandayan, a professor and coordinator of Plastic Surgery for the Department of Surgery at the School of Medical Sciences (FCM/Unicamp), a member of Biofabris. In addition to the convergence of interests in lines of research, there was the physical proximity of their laboratories. “It was an afternoon of conversations in which I explained my needs in the medical field and they set out to find solutions to meet my requirements.” As time passed and the Institute grew, more questions and proposals arose. “We now hold weekly meetings and each discussion generates new ideas.”
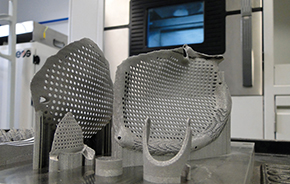
CAIUS LUCILIUS/HC-UNICAMPCraniofacial prostheses made of titaniumCAIUS LUCILIUS/HC-UNICAMP
Manufacturing the three customized titanium implants comprising the prosthesis, consisting of a 10 cm long surface, took 20 hours. The first step in manufacturing a prosthesis is to use tomography to make images of the area of the body requiring repair. These images are placed in the InVesalius program, a software developed by CTI, which is responsible for reconstructing the affected part in 3D. Based on a comparison of the intact part and the part affected by trauma or accident, the researchers create a prosthesis on the most appropriate scale and format, preserving the appearance and restoring the original function of protecting the brain. Based on this virtual model of the patient’s head, a skull model and a nylon prosthesis for 3D printing are then made. “The virtual planning is a time-consuming step, in which the programmer and the medical team discuss any necessary adjustments before arriving at the final metal prosthesis,” says Kharmandayan.
Finishing and sterilization
In the final step of manufacturing the metallic prosthesis, an alloy with titanium powder is placed in the additive manufacturing machine, a printing technique in which a three-dimensional model is created by successive layers of material. The powder is sintered by laser to form layers measuring 0.4 millimeters. Depending on the type of piece, its manufacture can take up to one day for the process to be completed. Once removed from the machine, the piece is given a thermal or chemical treatment and, if for use in medical implant applications, it will undergo a cleaning process and surface finishing for removal of residues and sterilization.
Jessica was the sixth patient operated on by the Kharmandayan team. She is one of the patients who is part of a project approved by Unicamp’s Ethics Committee, which calls for 15 surgeries. “It was the first craniofacial surgery we did with the material. The others were just the skull or face,” says Kharmandayan. The first patient was operated on in 2012, with the placement of a prosthesis to reconstruct the skull of a 17-year-old, three years after a serious bicycle accident. “He had stopped studying, was confined to the house, and had no social life. After the surgery, he went back to school, started playing the guitar, got engaged, obtained a driver’s license and went on to pass a civil service examination.”

INCT-BIOFABRISDesign of the prosthesis based on the 3D modelINCT-BIOFABRIS
The treatment now most widely used to restore the affected area is to remove a bone segment from the healthy side of the head and place it in the traumatized area. But this is not always possible. “When defects are large or when bone absorption occurs because of infection, one has to resort to a synthetic, metal or non-metal replacement,” Kharmandayan explains. One of the materials most frequently used for this purpose is methyl methacrylate, a type of plastic discovered in the 1920s. “There have been several reports of patients whose systems rejected the prosthesis because the material can release chemical substances.” Another aspect is that reconstruction using methyl methacrylate is done by hand by the surgeon. “The plastic in the form of paste, at a temperature of 82° Celsius, is shaped directly over the patient’s skull in the case of a cranial reconstruction.” Shaping by hand leaves much to be desired. Among the patients operated on at Unicamp’s Hospital as part of the project, four had previously had prostheses made from plastic.
Titanium alloys have long been used in medicine and, some years ago were used in dental implants—titanium is a material already well tested, safe and one that does not subsequently release residues. “In addition to being safe, the mini-plates we use allow integration with bone,” says Kharmandayan. “Their surfaces are manufactured with small grooves, so that bone integration and cell growth occur more rapidly than on an ordinary surface,” says Maciel. Titanium plates for craniofacial reconstruction are produced by other countries and sold in the market, but they are made in a standard size, and not tailored to patients and their needs. “A plate like the one implanted in Jessica would cost around R$130,000 in the market,” says Maciel. “The expenses we incurred for the material to build a customized plate and plates used by other patients cost around R$3,000 to R$5,000, depending on the material used.” This does not include medical fees and machine acquisition costs, design and sterilization, for example, which have been absorbed by Biofabris.

ANTONIO SCARPI NETTISkull study model and prosthesisANTONIO SCARPI NETTI
New Materials
In addition to the prosthesis customized with titanium alloys, other lines of research involving the search for new materials are developed with partner institutions. One line of research, in collaboration with UFRGS, focuses on calcium phosphate bioceramics, such as hydroxyapatite a material similar to the mineral part of bone, as well as other parts of the bone. “We do the synthesis and characterization of ceramics and we shape the pieces in rapid prototyping equipment,” says Cecilia Zavaglia, a professor in the Department of Materials Engineering, School of Mechanical Engineering (FEM), and deputy coordinator of the Institute. The ceramics we developed, known as beta tricalcium phosphates, may be used as replacement bones and teeth, in minor repairs. Tests in vitro and in vivo have been performed to evaluate the biocompatibility of the material and its toxicity. The next step will be clinical trials.
Other materials used in biomanufacturing are biopolymers. Molasses from sugarcane, açaí seeds and castor oil are raw materials from renewable sources used to manufacture these materials. From molasses, for example, researchers have obtained polylactic acid, a polymer absorbed by the body at controllable rates. “We polymerize lactic acid to use as a base for a number of applications such as tissue regeneration, artificial skin, and formation of cartilage and bone,” says Jardini. “This material can be used like a scaffold for seeding cells that need to be developed in a particular location.” The polymer is processed on a 3D printer to acquire the proper format for implantation in the patient. This biopolymer is then seeded with the patient’s own cells and, after growth, the prosthesis can be implanted in the desired location.
A polyurethane was developed from açaí seeds to be used as a bone prosthesis, especially in the skull and facial areas (see Pesquisa FAPESP Issue nº 196). And castor oil associated with citric acid has resulted in a new polymer, which led to a patent filing. “The castor oil was subjected to a reaction with citric acid, which resulted in a cross-linked polyester obtained from a polymerization process that did not involve toxic agents to induce the chemical reaction,” says Maria Ingrid Rocha Barbosa Schiavon. She initiated the research during her postdoctoral work, which resulted in a joint patent filing with other Biofabris researchers.
from the polylactic acid obtained from sugarcane, in combination with poly 2 hydroxyethyl methacrylate (pHEMA), a hybrid polymer was formed as a result of the doctoral research of Marcele Fonseca Passos, under the advisorship of Maciel and Carmen Gilda, of the Department of Mechanical Engineering, at the Federal University of Pará (UFPA). The research led to a patent filing. The process does not require chemical agents and the product obtained has the potential to be used in dentistry, and for the partial regeneration of meniscus and ear cartilage. Cytotoxicity tests showed the polymer’s biocompatibility and it is now being tested on animals at the UFPA School of Biology in collaboration with the Evandro Chagas Institute, also in the state of Pará.
Projects
1. Biofabris – Institute of Biomanufacturing (nº 2008/57860-3); Grant Mechanism: Thematic Project – INCT; Principal Investigator: Rubens Maciel Filho (Unicamp); Investment: R$2,691,894.52 (FAPESP) and R$2,239,094.33 (CNPq).
2. Epoxy biopolymer synthesis from renewable sources for building biomedical devices using rapid prototyping techniques and biomanufacturing (nº 2009/16480-6); Grant Mechanism: Scholarships in Brazil – Post-doctoral degree; Principal Investigator: Rubens Maciel Filho (Unicamp); Grant Recipient: Ingrid Maria Rocha Barbosa Schiavon; Investment: R$215,732.36 (FAPESP).
3. IPNs networks of pHEMA-PLA for use in tissue engineering (nº 2011/18525-7); Grant Mechanism: Scholarships in Brazil – Doctorate; Principal Investigator: Rubens Maciel Filho (Unicamp); Grant Recipient: Marcele Fonseca Passos; Investment: R$177,978, 84 (FAPESP).
Scientific articles
CALDERONI, D.R. et al. Paired evaluation of calvarial reconstruction with titanium implants prototyped with and without ceramic coating. Acta Cirúrgica Brasileira. V. 29, p. 579-87. 2014.
JARDINI, A.L. et al. Cranial reconstruction: 3D biomodel and custom-built implant created using additive manufacturing. Journal of Cranio-maxillo-facial Surgery. V. 42, p. 1877-84. 2014.
LAROSA, M.A. et al. Microstructural and mechanical characterization of a custom-built implant manufactured in titanium alloy by direct metal laser sintering. Advances in Mechanical Engineering. V. 2014. p. 1-8. 2014.