 LÉO RAMOSThis is bad news for those who like to sunbathe, even if they slather on the sunscreen. Sunscreens now available on the market protect against the effects of ultraviolet radiation, which is invisible to the human eye, but they cannot prevent the damage caused by visible light. And this damage can be severe. A study conducted by São Paulo and Paraná researchers has just demonstrated that visible light can also cause skin cancer, the most common form of cancer in Brazil, which accounts for 25% of cases of malignant tumors, according to Brazil’s National Cancer Institute.
LÉO RAMOSThis is bad news for those who like to sunbathe, even if they slather on the sunscreen. Sunscreens now available on the market protect against the effects of ultraviolet radiation, which is invisible to the human eye, but they cannot prevent the damage caused by visible light. And this damage can be severe. A study conducted by São Paulo and Paraná researchers has just demonstrated that visible light can also cause skin cancer, the most common form of cancer in Brazil, which accounts for 25% of cases of malignant tumors, according to Brazil’s National Cancer Institute.
Maurício Baptista, a biochemist at the University of São Paulo (USP) and the study’s coordinator, is not surprised by this finding, which was published in the November 2014 issue of the journal PLOS One. Indeed, from a physical standpoint, the light the human eye can see and ultraviolet (UV) rays have much in common. Both come from the same form of energy, electromagnetic radiation, which, based on the intensity has different names—gamma rays, X-rays, visible light and infrared radiation. “To skin, the distinction between visible and invisible light is arbitrary,” says Baptista, a professor at USP’s Chemistry Institute and a researcher at the National Institute of Science and Technology in Redox Processes in Biomedicine (INCT-Redoxoma).
He and his team have shown that visible light can damage the genetic material (DNA) of the cells indirectly by interacting with melanin. This dark pigment, which is responsible for skin color, absorbs some of the energy of visible light and transfers it to oxygen molecules, generating highly reactive forms—the so-called singlet oxygen. This excited oxygen molecule, in turn, reacts with organic molecules, such as DNA, and degrades them. When this type of damage affects a regulatory gene of cell proliferation, the cell can begin to multiply uncontrollably, causing cancer.
This finding can help us to better understand the origin of some forms of skin cancer. “The group’s contribution, which is very rigorous in scientific terms, helps us to understand the mutation profiles we found in human melanomas, where evidence of DNA oxidation events is often observed,” says Dr. Roger Chammas, a professor at the University of São Paulo School of Medicine and a researcher at the São Paulo State Cancer Institute. “In the past these events were attributed to UVA radiation, but, now, as it turns out, it could also be the effect of visible light.”
The mechanism producing these more reactive molecules observed by Baptista’s group confirms melanin’s dual role: it protects the skin from damage caused by certain types of light, while at the same time facilitating the damage caused by others. Like the current experiment, previous studies have already shown that exposure to ultraviolet type B (UVB) rays made the melanocytes, melanin-producing cells, increase their synthesis of the pigment. They have also shown that a greater proportion of these cells survived under this form of radiation. The mortality rate, however, was much higher when more pigmented cells were subjected to ultraviolet type A (UVA) radiation, something similar to what is now occurring under visible light.
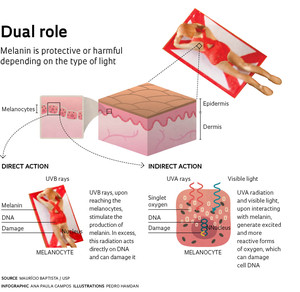 The protection that melanin offers against UVB rays is not enough to prevent skin cancer however. This form of radiation, associated with sunburn, an acute inflammatory response to excessive exposure to sunlight, was the first proven to be able to cause cancer. It penetrates the skin slightly, but what is not absorbed by melanin goes directly to the DNA—especially that of the melanocytes—and can damage it and cause a rare and very aggressive form of cancer: melanoma, which is more common in adults with a fair complexion and represents 4% of the malignant skin tumors found in Brazil.
The protection that melanin offers against UVB rays is not enough to prevent skin cancer however. This form of radiation, associated with sunburn, an acute inflammatory response to excessive exposure to sunlight, was the first proven to be able to cause cancer. It penetrates the skin slightly, but what is not absorbed by melanin goes directly to the DNA—especially that of the melanocytes—and can damage it and cause a rare and very aggressive form of cancer: melanoma, which is more common in adults with a fair complexion and represents 4% of the malignant skin tumors found in Brazil.
Yet the penetration of UVA radiation, which like visible light causes DNA damage through the production of excited and more reactive forms of oxygen, goes deeper. In the 1980s it was discovered that UVA rays caused another form of cancer—known as non-melanoma, which is more common after age 40—originating in the so-called basal or squamous cells. Some time after the harmful effects of UVA and UVB rays were proven, the pharmaceutical industry developed compounds that effectively block these two bands of radiation. But now we are beginning to see that this may not be enough. “Sunscreens only protect against ultraviolet rays, so the information about what protects the skin is incomplete,” says Baptista. “One important aspect is the regulation of packaging and advertising, so as not to disseminate misleading information.” This, incidentally, is an issue yet to be resolved. Baptista recalls the case of UVA radiation. Although its harmful effect had been established for about 30 years, it was only in 2013 that manufacturers were required to specify on the packaging if the product protected against one or both types of UV radiation.
Baptista obtained the first evidence that visible light could also be harmful in 2011, when tests showed that singlet oxygen appeared when it interacted with pure melanin or the melanin found in hair. “The discovery of the harmful effects of UVA a few decades ago shattered the dogma that UVB was the only band of the solar spectrum that caused damage to the skin,” says Baptista. “Now we need to shatter the dogma that these harmful effects are only due to UV rays.”
To fully demonstrate the carcinogenic effect of visible light, however, there is at least one more step still needed. It must be shown that the DNA damaged by visible light leads to profound genetic changes (mutations). “Tests will need to be done on animals and then in humans, and if confirmed, this will be an important discovery,” says Dr. João Duprat Neto, an oncology surgeon and director of the Skin Cancer Center of the A.C. Camargo Cancer Center. “It is possible that this data will stimulate the development of more effective skin protectors.”
While waiting for sunscreens that also filter out visible light, the best way for people to protect against skin cancer is to avoid overexposure to the sun. But only if excessive, because there is another factor to be considered: sunlight is essential for the skin’s ability to synthesize vitamin D, which is important in the fight against osteoporosis and other bone diseases. According to Dr. Marco Antônio Oliveira, a dermatologist, also at the A.C. Camargo Skin Cancer Center, those who have a higher risk of developing skin cancer should replace sun exposure with vitamin D supplementation; the body’s production of vitamin D drops after age 40 along with aging of the skin. “It’s important to remember that the use of sunscreen is essential,” says Dr. Oliveira. “In the younger generations, which are better informed about the effects of the sun and use more sunscreens, the incidence of cancer has dropped significantly.”
Projects
1. Photosensitization in the life sciences (No. 12/50680-5); Grant mechanism: Thematic Project; Principal investigator: Maurício da Silva Baptista (Chemistry Institute/USP); Investment: R$3,067,571.88 (FAPESP).
2. Redoxoma (No. 13/07937-8); Grant mechanism: Research, Innovation and Dissemination Centers (RIDC); Principal investigator: Ohara Augusto (Chemistry Institute/USP); Investment: R$20,674,781.25 (for the entire project) (FAPESP).
Scientific article
CHIARELLI NETO, O. et al. Melanin photosensitization and the effect of visible light on epithelial cells. PLOS One. November 18, 2014.