Now in operation for nearly two decades, Brazil’s Mobile Emergency Medical Service (SAMU), an important patient access to treatment within the Unified Health System (SUS), has just received its first performance evaluation via a nationwide survey. According to a survey carried out by nurse Marisa Malvestio, a researcher in the postdoctoral program at the School of Nursing at the University of São Paulo (EE-USP), the public ambulance service people activate by dialing 192 has become a microcosm of both the great accomplishments and the difficulties with the SUS services overall.
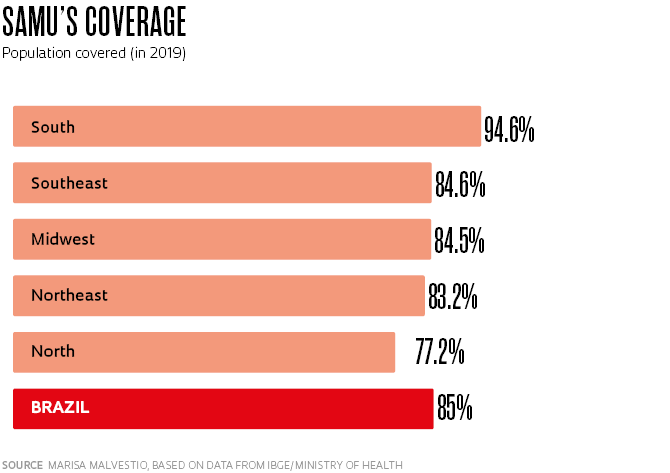
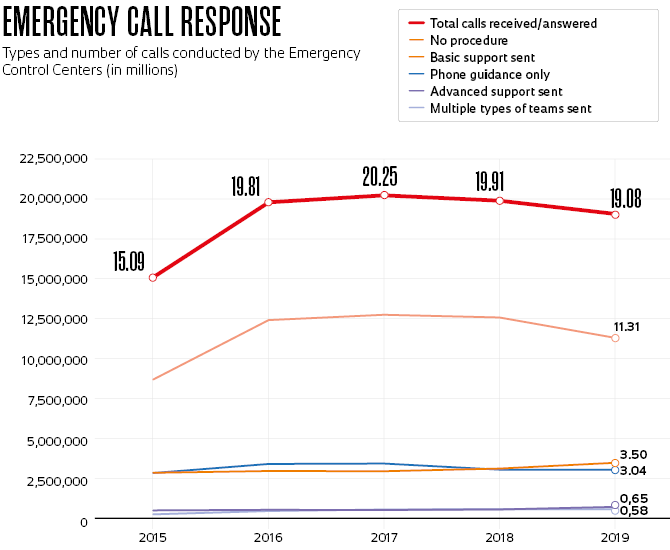
SAMU was the first concrete result of the National Emergency Policy, created in 2003, and currently assists 85% of the population in 67.3% of the country’s municipalities. In 2019, its services were requested by phone calls from more than 19 million Brazilians. This resulted in almost 4.3 million emergency response calls made by ambulances, mobile ICUs, and, to a far lesser extent, helicopters, boats, and motorcycles—approximately one medical response for every four emergency calls.
However, these extraordinary SAMU call numbers hide a persistent inequality in the service it provides. In an article published in July 2022 in the journal Ciência & Saúde Coletiva, Malvestio and her supervisor, Regina Márcia Cardoso de Sousa, a professor at EE-USP, gathered data from the Ministry of Health and the Brazilian Institute of Geography and Statistics (IBGE) and showed that, although coverage increased by more than 5% during the period from 2015 through 2019—reaching 178 million Brazilians—there are still areas with no SAMU emergency assistance or where the few available ambulances are shared by several municipalities.
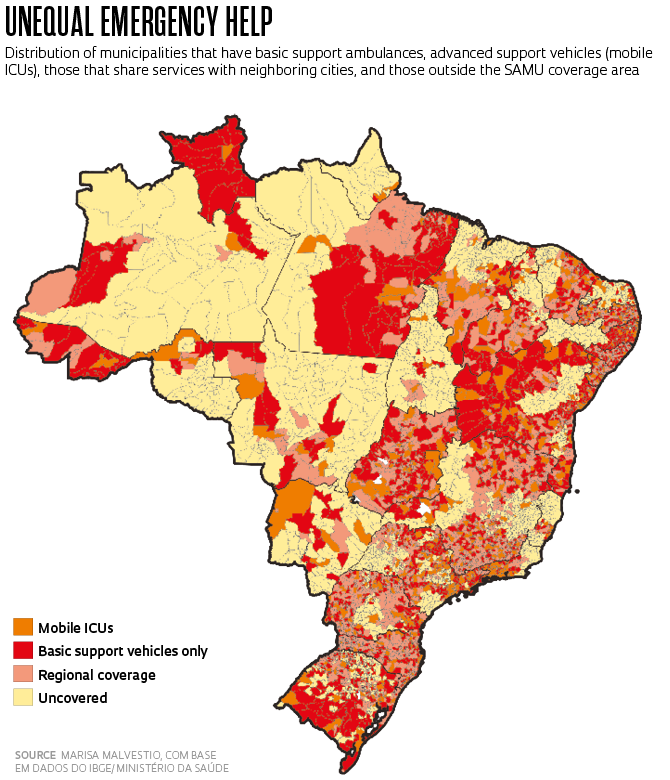
In 2019, there were 1,820 cities with no SAMU service, mainly in Brazil’s northern region. There are exceptions, such as the states of Roraima and Acre, which have good basic ambulance coverage but where few mobile ICUs are available. In 1,938 cities, SAMU service was being provided by municipal consortia, in accordance with the SUS system of regionalizing medical attendance. “This is a cruel system, since an ambulance may be 90 kilometers away from the place where the call is made,” explains the researcher, who has worked in prehospital emergency ambulance care in the city of São Paulo since 1990 and became a part of the team implementing SAMU beginning in 2003.
Malvestio’s postdoctoral research led to two other studies, which have been published in the SciELO Preprints repository and are currently under evaluation by scientific journals. One of the studies shows how the SAMU workforce evolved, growing 14% from 2015 to 2019, and mobilizing 41,400 professionals, including doctors, nurses, nurse technicians, emergency call operators, ambulance drivers, and support personnel. SAMU’s human resources are clearly insufficient for operating the 3,648 vehicles available. For the basic emergency ambulances that get sent out on less complex cases, the current contingent of nurse technicians and emergency response drivers can only utilize a maximum of 67% of the vehicle availability. For advanced emergency support vehicles, made up of mobile ICUs, there are enough doctors for only 36% of the fleet. Thus, nurses, with or without the assistance of nurse technicians, end up working in advanced support ambulances without the accompaniment of physicians in about 60% of ambulance calls.
Malvestio points out that on average SAMU ambulances arrive within approximately 30 minutes. “This is insufficient for the worst emergency, cardiorespiratory arrest, which requires professional treatment within six minutes. Even though these limitations create increased risk for many patients, SAMU saves lives every day and has a passionate workforce. The SUS National Force (for disaster response), which is now assisting with the Yanomami health emergency in Roraima, consists primarily of professionals from SAMU who volunteered for this mission,” she says.
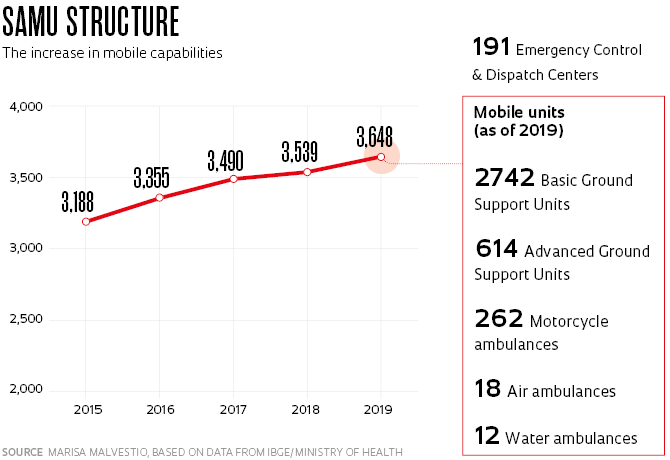
The researcher notes that the other preprint study found that the number of ambulance calls increased by 28.5% from 2015 to 2019. “With an aging population, the demand for emergency services increases greatly. This is already the case in many other countries and is beginning to happen in Brazil as well,” she adds.
The basic emergency response units each conduct on average 3.3 calls per day, while the mobile ICU units respond to 2.7. “The international average is seven patient response calls per day. In England’s system, it’s as high as 11. We probably only do 3.3 calls because many of the mobile resources don’t have teams to operate them 24 hours a day or they cover very large areas, which leads to long travel times, among other reasons,” she suggests. Dialing 192 gives the caller access to an emergency and urgent call control center, where telephone operators answer calls and pass them on to professionals with medical training. The physicians then identify the urgency of the situation, make a primary diagnosis, and determine the emergency priority and which type of mobile resource should be sent—a regular ambulance or a mobile ICU.
The cost of the system should be tripartite, with the federal government paying 50% of the costs. The Ministry of Health annually transfers around R$1.3 billion to states and municipalities, who are then supposed to divide the other 50%. In practice, other governmental agencies have been covering the municipalities’ share. “The Ministry of Health determines how the service should be organized, allocates funding and investment, and distributes and oversees the ambulances, but operations, management, and decision-making power rests with the municipality—or a group of them, associated in consortia,” Malvestio says.
Physician Gisele O’Dwyer, a researcher at the Oswaldo Cruz Foundation’s National School of Public Health (ENSP-FIOCRUZ), says that one of the merits of Malvestio’s investigation is to present an overall analysis of the SAMU system. “Several regional studies have been carried out, but they’re incomplete because the country is so diverse. There are very fragile services throughout Brazil,” says O’Dwyer, who coordinated research on the implementation and location siting for the SAMU services in the state of Rio de Janeiro during the early 2010s. The absence of a universal and uniform system frustrated one of SAMU’s initial ambitions, which was to become a major public health observatory. “The idea was that if we knew what the problems were, their severity, and where they occurred, it would be possible to understand Brazil’s main public health challenges and prepare the SUS to face them,” says O’Dwyer.
There are two principal models of emergency ambulance care used around the world. One of them, from the United States, works based on sending a type of medical professional trained in prehospital urgent care, the paramedic. The other, which to a certain extent inspires the Brazilian experience, is the current model used in European countries. “In France, emergency response vehicles must have a doctor, which makes the service much more expensive,” says Marisa Malvestio. The French system, implemented in 1986 under the name Service d’Aide Médicale Urgente, was where Brazil’s system borrowed the acronym SAMU. “In other countries, such as England and Sweden, there are more nurses, which makes it possible to care for more people,” she says.
Dr. Oswaldo Tanaka, from the Department of Politics, Management, and Healthcare at the School of Public Health (FSP) at USP, says that the fact that most ambulance calls are conducted by nurses and nurse technicians is not a problem. “They are very well trained to follow protocols that aim to shorten the assistance time, save lives, and prevent sequelae,” he explains. He observes that under the current SUS funding conditions, it would be difficult to significantly increase the number of physicians available for mobile emergency care. “We have to think about ways to improve our ability to make diagnoses and get to the hospital quickly,” he says.
This is not, of course, a trivial task. Tanaka classifies the difficulties faced by the service as a “wicked problem,” an expression used to classify problems that are very difficult or even impossible to solve and that are based on unstable, complex, or contradictory premises. “SAMU is perhaps the most complicated part of the SUS administration. It has to be prepared for any emergency that affects anyone at any time and provide the best possible response in the shortest amount of time,” explains Tanaka, who, in the mid-2010s studied SAMU performance in the city of São Paulo, together with his doctoral fellow Flávia Saraiva Leão Fernandes, now a professor at the Federal University of São Paulo (UNIFESP). This study discovered an apparent contradiction: in situations involving mobile ICUs, which arrive with a doctor and advanced support equipment, a significant number of cases resulted in death. “Many cases were quite complicated and, even with all their efforts, the worst outcome couldn’t be avoided.”
In Tanaka’s assessment, Malvestio’s studies contribute to understanding the different challenges facing SAMU, however, to improve the service it would be necessary to pursue metrics beyond the traditional measurements. “In my view, data on population and territorial coverage aren’t very helpful in planning medical attendance. The starting point should be the emergency calls received by 192—how many involve traffic accidents, or fractures, cardiac syncope, epileptic seizures, and problems related to early discharge from surgeries and drug addiction,” says Tanaka. “We need to evaluate when they happen and how many were resolved. Even the day of the week and traffic conditions at the time of the emergency are important for planning.”
By all measures, the SAMU system has been essential in saving lives, as has already been proven in the researcher’s own life. On August 17, 2021, Tanaka, then the director of FSP-USP, was participating in a virtual meeting with other professors to discuss the return to in-person activities, when a colleague questioned him. “Your voice is getting thick,” he heard. Then the other professor said: “You look like you’re having a stroke. Lie down on the floor right now.” Alone at home, Tanaka obeyed, lost consciousness, and woke up in a hospital. He remained in the ICU for several days and is still recovering from the incident. “I was saved by SAMU. The speed with which the help arrived was crucial,” he says.
Emergency Control Center (CRU)
The #192 phone attendance responsible for receiving, evaluating, and dispatching emergency calls
Mobile Resources
Basic or advanced support ambulances, motorcycle ambulances, boats, air ambulances
Basic Ground Support Unit
Ambulances for less complex patient care
Advanced Ground Support Unit
Mobile ICUs used to transport high-risk patients in prehospital emergencies or between hospitals. They travel with one doctor and a nurse, in addition to the ambulance driver
Motorcycle ambulance
Motorcycles driven by nurses or nurse technicians trained for rapid access and providing care in places other ambulances cannot reach
Water ambulance
Medical service units for populations where access is only possible by river. Basic support boats are crewed by a driver and a nurse technician. Advanced support units are required to have a doctor and a nurse
Air ambulance
Emergency care provided by doctors and nurses trained to operate via helicopter or plane
