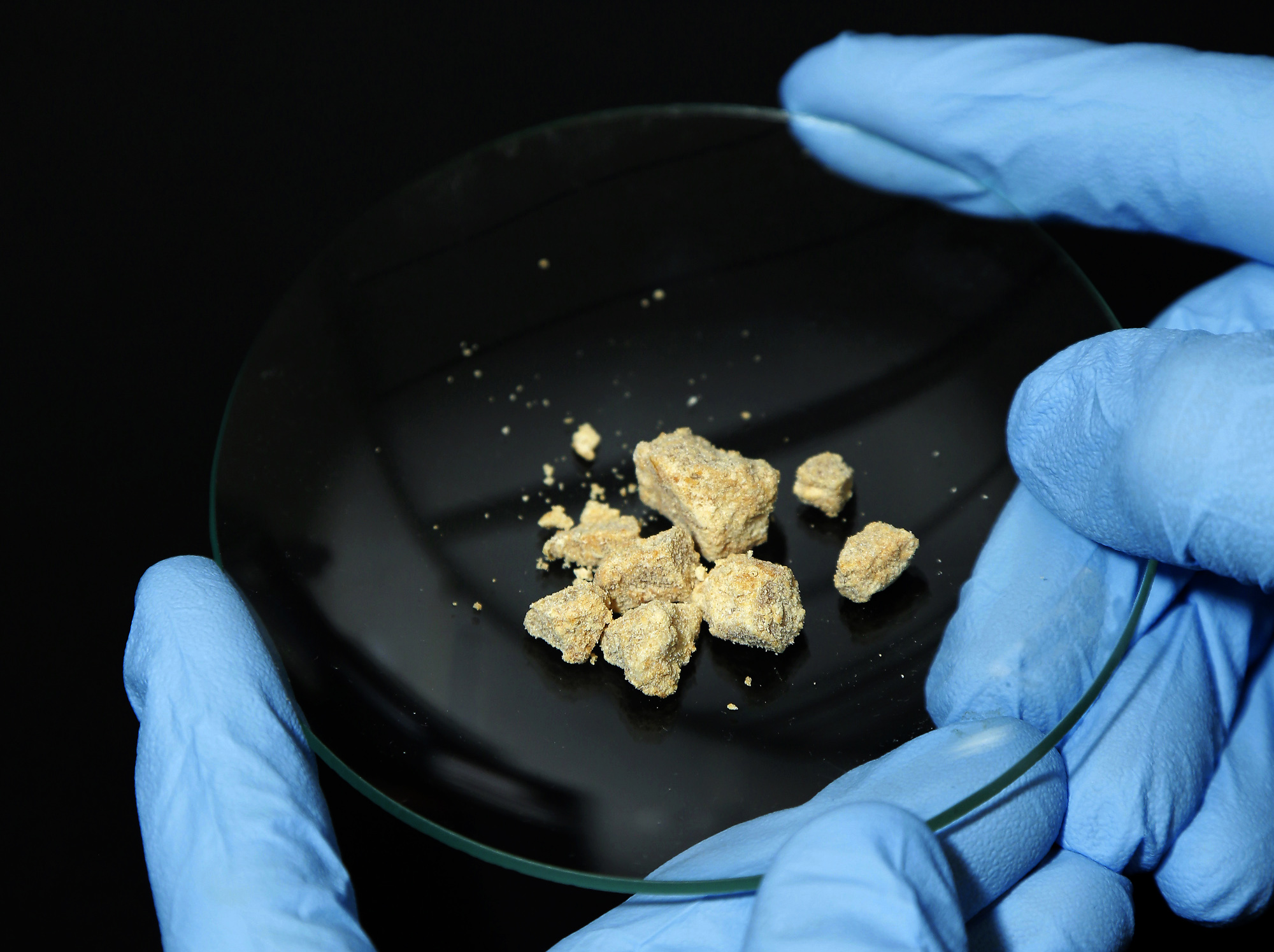
Foca Lisboa / UFMGCocaine base: cocaine is the second most consumed illicit substance in BrazilFoca Lisboa / UFMG
Addiction to cocaine, including its derivatives such as crack, remains a global public health concern for which the medical community has yet to find an effective treatment. A team of researchers at the Federal University of Minas Gerais (UFMG) is turning to immunology to find a solution. The group is developing a novel vaccine against cocaine addiction and is currently seeking funding for its first human trials. Initial experiments on animals have demonstrated the ability of the vaccine to stimulate the production of anti-cocaine antibodies, but scientific evidence confirming its effectiveness in reducing drug dependency has yet to be obtained. The researchers plan to conduct further testing in animals before proceeding to clinical trials involving human volunteers on a to-be-determined date.
“In testing on rodents and nonhuman primates — specifically of the species Callithrix penicillata — our vaccine, called Calixcoca, produced no significant side effects. We only observed a mild reaction at the injection site, which did not affect the overall health of the animals,” says Frederico Duarte Garcia, a professor in the Mental Health Department at the UFMG School of Medicine and the lead author of the study.
The name Calixcoca, he says, is inspired by the chemical structure of the immunizing agent, known as calixarene, so named because it resembles a chalice. This molecule serves as the carrier for the antigen, a hapten that is an analog of cocaine — carriers are high-molecular-weight substances that are capable of eliciting an immune response.
Pharmacist Paulo Sérgio de Almeida Augusto, a member of the UFMG research group, explained that haptens are tiny molecules that, due to their diminutive size, are typically not recognized by the immune system as invaders; therefore, haptens need to be combined with larger carrier macromolecules to prompt an immune response within the body. This is the case with cocaine. Augusto explains, “Cocaine represents a foreign molecule within the human body. However, it often lacks the molecular weight and chemical complexity required to elicit a substantial immune response. Although such a response may occur in individuals who frequently use high doses of the drug, it does not occur in every individual.”
The researchers developed their immunizing agent by deriving a hapten from a cocaine molecule specifically modified to bind to the carrier. When coupled with calixarene, the derived hapten has a higher molecular weight and is able to elicit an immune response. If a vaccinated individual uses cocaine or crack, the antibodies will bind to the drug molecules in the bloodstream, preventing — or at least reducing — their passage through the blood–brain barrier. This barrier lines the blood vessels that vascularize the central nervous system, acting as a selective gatekeeper that controls the transport of substances into the brain.
In mice administered with the synthesized molecule, radiochemical assays conducted by UFMG researchers showed that the vaccine successfully reduced drug transport across the blood-brain barrier. “Immunized animals were treated with a radiolabeled analog of cocaine. Immunosorbent assays showed a lower concentration of this compound in the brain and a higher concentration in the bloodstream compared to those in animals that received only the placebo,” explains Augusto. The study results were published in the Journal of Advanced Research.

UFMGRadiochemical essay images showing a lower concentration of a radiolabeled cocaine analog in the brains of rodents immunized with the UFMG vaccine (pink dots in the center of the image) compared to the control groupUFMG
The UFMG researchers hypothesize that if the vaccine is able to prevent cocaine molecules from crossing the blood-brain barrier, individuals will no longer experience the same pleasurable sensations that previously triggered the brain’s reward circuitry, driving compulsive behavior. This, however, has yet to be demonstrated in clinical trials. “Without the compulsion, patients have the opportunity to reclaim their family life, pursue their professional interests, and rediscover their other pleasures and interests that were once overshadowed by addiction,” explains Garcia.
Long-standing challenges
The new therapeutic approach is viewed with guarded optimism by drug addiction experts. “The medical field has yet to develop an approved drug for fighting addiction. Current treatments primarily focus on managing the symptoms of withdrawal and related disorders, coupled with behavioral therapy,” explains Fábio Cardoso Cruz, a professor of biochemistry in the Department of Pharmacology at the Federal University of São Paulo (UNIFESP) who was not involved in the UFMG study.
Cruz is currently researching the neurobiological mechanisms underlying relapse to cocaine use in a FAPESP-funded project. His study aimed to answer the question of why 70% to 80% of individuals relapse during treatment. “This shows the urgent need to develop new therapeutic strategies. Vaccines are now emerging as a promising pharmacological approach,” he says.
Calixcoca is not the first immunology-based therapeutic formulation developed to treat substance dependence. “The therapeutic potential of vaccines against drug addiction was first demonstrated in the mid-1970s when a conjugate of morphine and bovine serum albumin was found to mildly reduce heroin self-administration in a rhesus monkey. The first papers describing attempts to develop vaccines against cocaine and nicotine addiction were published in the 1990s,” says Cruz. The rhesus monkey experiment was published in Molecular Psychiatry in 1974.

UFMGRaissa Pereira, a PhD student at UFMG, holding a vial containing the Calixcoca vaccine formulationUFMG
Despite the promising results in preclinical trials and some early clinical trials, no antidrug vaccines have yet been approved. “Several hurdles remain on the path to clinical success. Notably, not all individuals respond uniformly to these vaccines, and in some individuals, the levels of antibodies necessary for achieving the desired clinical efficacy may not be produced,” says Cruz from UNIFESP.
“In general, vaccines are shown to be efficient in animal models. However, when they progress to the clinical trial phase, the results often fall short of expectations,” says Denise Morais da Fonseca, an immunologist affiliated with the Institute of Biomedical Sciences at the University of São Paulo (ICB-USP). In March, she collaborated in developing an ICB course on pharmacological treatments for addiction. In preparation, she delved into the literature reviews concerning drug vaccines — obtaining rather disappointing results. “A 2022 review documented 23 clinical trials involving antidrug vaccines, with six targeting cocaine addiction — most were focused on nicotine,” notes Fonseca. “Every single one of them failed.”
Some vaccines, she elaborates, failed to elicit a sufficient quantity of antibodies, or the immune response waned far too quickly. The precise reasons behind these results remain unclear, although they might be attributed to genetic variability among the individuals tested — a factor absent in animal models. “In most studies, researchers use isogenic mice, meaning they are genetically identical,” Fonseca explains.
Another possible explanation could lie in the behavior of the vaccine recipients themselves. “In some unsuccessful trials, individuals struggling with addiction consumed larger drug doses to achieve the desired effect,” she remarks.
The UFMG researchers recognize the theoretical risk of individuals attempting to overcome the effects of the vaccine by consuming larger doses of cocaine to reactivate the brain’s reward circuitry. According to Augusto, this concern will be addressed in subsequent studies using experimental models that can estimate the quantity of the drug that the vaccine is capable of blocking. “Our primary goal is to roadblock the compulsion mechanism,” Garcia notes. “Beyond a certain point, increased consumption would significantly increase the cost for the user, to a point where it becomes financially prohibitive.”
The UFMG group is confident that Calixcoca will outperform the other vaccine candidates in terms of efficacy. The researchers’ confidence stems from the unique chemical composition of the vaccine. “The key distinction in our proposition is that the vaccine has no protein base. Calixarene is a synthetic organic substance,” says Ângelo de Fátima, a professor at the UFMG Department of Chemistry who developed the vaccine’s immunogenic platform.
Prior antidrug vaccine programs have relied on proteins as carriers, some of which have been used in other commercially available vaccines. This raised concerns about potential sensitization issues. “Patients reacted not only against the drug but also against these proteins. Our vaccine induces a better response because it introduces an entirely new molecule to the body,” Garcia says.
Another significant advantage of the new formulation, such as its developers, lies in its production process. “Calixarene is a more stable substance and doesn’t require a cold chain for production and storage. This makes the process more cost-effective,” Garcia explains. A cold chain refers to the logistics of handling, storing, distributing, and transporting temperature-sensitive medications.
Even if Calixcoca proves effective in generating antibodies against cocaine in humans in future clinical studies, additional therapeutic support will be needed, Cruz notes, drawing on his research into the biological mechanisms of addiction. He notes that patients’ associative memory related to drug use can be triggered by various cues, such as stress or exposure to environments and settings associated with drug use.
