 Léo RamosAt 74, Guido Carlos Levi, an infectologist from São Paulo, devotes part of his time to clearing up the doubts of people who are still suspicious about the benefits of vaccines. The week he was interviewed by this magazine at his office in the capital of São Paulo, he had done his utmost to convince an 85-year-old woman, who had never been vaccinated, to get a flu shot to protect herself from the H1N1 virus. She was accompanied by her husband, who had turned to the doctor in hopes that he could change her mind. The woman, who called vaccines “filthy poison,” eventually gave in to Levi’s explanations. “I told her that it had been thanks to vaccines that we’d been able to eradicate diseases like smallpox, which killed millions in Europe and the Americas,” he says. This rejection of vaccines is the theme of Recusa de vacinas – Causas e consequências (Refusing vaccines: causes and consequences), a book published by Levi in 2013. Historically, this kind of resistance has been associated with under-educated sectors of the public, but, according to the doctor, the profile has changed and it is now a phenomenon among the higher social classes. “This slice of the population has greater access to alternative treatments, like homeopathy or anthroposophic medicine, which often do not recommend vaccination.”
Léo RamosAt 74, Guido Carlos Levi, an infectologist from São Paulo, devotes part of his time to clearing up the doubts of people who are still suspicious about the benefits of vaccines. The week he was interviewed by this magazine at his office in the capital of São Paulo, he had done his utmost to convince an 85-year-old woman, who had never been vaccinated, to get a flu shot to protect herself from the H1N1 virus. She was accompanied by her husband, who had turned to the doctor in hopes that he could change her mind. The woman, who called vaccines “filthy poison,” eventually gave in to Levi’s explanations. “I told her that it had been thanks to vaccines that we’d been able to eradicate diseases like smallpox, which killed millions in Europe and the Americas,” he says. This rejection of vaccines is the theme of Recusa de vacinas – Causas e consequências (Refusing vaccines: causes and consequences), a book published by Levi in 2013. Historically, this kind of resistance has been associated with under-educated sectors of the public, but, according to the doctor, the profile has changed and it is now a phenomenon among the higher social classes. “This slice of the population has greater access to alternative treatments, like homeopathy or anthroposophic medicine, which often do not recommend vaccination.”
Levi holds a doctorate in medicine from the University of Campinas (Unicamp), where he taught at the School of Medical Sciences. He also sits on the technical committee of Brazil’s National Immunization Program, launched in 1973 and run by the Ministry of Health. “The program is a model worldwide. Average vaccine coverage in Brazil is more than 95%, with free doses available at over 35,000 public health clinics,” he explains. As a public servant, Levi headed the Emílio Ribas Institute of Infectology from 1995 to 2001. He currently serves as director of the Brazilian Immunization Society and is one of the founders of CEDIPI, a private clinic founded in São Paulo in 1972 that provides vaccines, some of which are not yet available through Brazil’s public health system, such as the one against shingles. In this interview, Levi talks about the problem caused by people refusing vaccines and about research into new immunizations.
| Age |
| 74 |
| Specialty |
| Infectology |
| Education |
| Graduate of the sorocaba school of medicine (PUC) and Phd in medicine from the university of campinas (Unicamp) |
| Scientific production |
| Author of more than 100 scientific articles; wrote or edited some 40 books |
How did you become interested in vaccines?
I did my residency at the São Paulo State Public Servant Hospital in the 1960s and took part in an initiative there at the invitation of Professor Vicente Amato Neto. It involved volunteer work in poor communities in the Serra do Mar mountain range, where there was no access to basic sanitation. There were thousands of people who had diseases that could be treated with simple anti-parasitics. And there were other ailments that could have been avoided through vaccination. We set up mobile clinics, and one of the main initiatives was to vaccinate children. The hospitalization rate for those people fell about 90%. Our team grew and we started providing care at other locations on the outskirts of São Paulo. This experience also resulted in the publication of scientific papers in the fields of parasitology, immunization, and public health.
You’ve written a book about refusing vaccines. How big a problem is this?
A lot of inaccurate information gets spread around the internet, and this confuses people. In the case of vaccines, it’s common to find incorrect information about their side effects, which influences people’s decisions to be immunized or not. One example: the vaccine against the influenza A virus [H1N1] – swine flu – doesn’t contain mercury, like people say. Mercury is used in microscopic doses as a preservative, only in vaccines that are available in 10-dose vials. Individual vaccines, like the one against H1N1, don’t contain any. And there is research showing that even in vaccines that do contain mercury, the amount present isn’t toxic. Yet there are still folks who claim the flu shot is bad for you because it contains mercury.
In addition to the lack of information, haven’t there been some cases involving bad faith?
Yes. One of the most emblematic cases involved Andrew Wakefield, a former British researcher who published a paper in the journal The Lancet in 1998, allegedly linking the MMR vaccine to autism in 12 children. According to Wakefield, this happened because essential vitamins and other nutrients were poorly absorbed, which, at the same time, facilitated the absorption of proteins that could cause encephalopathy and thus occasion autism. The study was criticized, and since the authors were prominent in their fields and there was a big stir, a number of investigations were carried out to confirm the veracity of the findings. Research conducted in various places, like the United States and Asia, found no relation between the vaccine and autism. Then it was discovered that Wakefield had received a kickback from a law firm that was interested in suing laboratories and doctors. In 2010, The Lancet retracted the paper, which was deemed fraudulent. Wakefield was taken to court in the United Kingdom and lost his license in 2014.

Personal archives
In 1957, Levi (center, in black) played goalie for the Dante Alighieri High School soccer team, in São PauloPersonal archivesIs this resistance to vaccines found among a specific segment of the population?
This resistance is curious. Right now, we see that it is a phenomenon among the higher and more intellectualized classes. A team from the University of São Paulo (USP) has done a study reinforcing this thesis. In more recent times, anti-vaccine movements have lost a great deal of the religious base they had in the past. People in the upper classes have more access to alternative treatments and to homeopathy and anthroposophic medicine, which often do not recommend vaccination. Homeopaths are split between those for and those against vaccines. No classic scholar of homeopathy has opposed vaccination. Samuel Hahnemann himself, the father of homeopathy, was an enthusiastic advocate of the smallpox vaccine. Nonetheless, there are a lot of homeopaths who don’t recommend it. On the other hand, in anthroposophic medicine – a philosophical and mystic philosophy founded in the early 20th century by Rudolf Steiner, an Austrian – there’s a stance against vaccination, although we don’t find any literature that either favors or opposes immunization. There’s also the Christian Science community, which was founded in the United States, where a case of measles appeared in 1994 and triggered an epidemic in Missouri and Illinois. This group bans the use not just of vaccines but of any kind of medicine, grounded in the argument that “no one can defy the will of God.”
These are small groups. Do they wield much influence?
They are indeed minorities. The problem is that when one person gets a vaccine, he’s not protecting only himself but his community as well. If one group – no matter how small – fails to be vaccinated, there’s a chance an outbreak will be triggered and affect people who haven’t been vaccinated yet. In 2011, for example, there was a measles outbreak in São Paulo, which began at a school that followed the anthroposophic philosophy, in the neighborhood of Butantã, where a lot of parents had opted not to vaccinate their children. This line of thought believes that a healthy diet is enough to keep children healthy.
Some people claim that too many vaccines can overload the immune system. Is there any evidence for this?
There are scientific controversies, but it must be made clear that there’s often no science behind many arguments. The physician Robert Sears, author of the best-seller The vaccine book: Making the right decision for your child, published in 2007, suggests that current vaccine schedules overload the immune system because they call for the administration of combination and multiple vaccines. This is supposedly further aggravated by an excess of aluminum, albumin purified from human blood, and thimerosal, a substance used to preserve medicine. Sears proposes an alternative schedule that spaces vaccines out more, in separate applications. But if you do a more thoroughgoing analysis of Sears’s book, you won’t find any research backing up these conclusions. There’s nothing. When he states that the MMR vaccine contains albumin purified from human blood, he shows he doesn’t know that this product is obtained from tissue cultures and not from blood. Some arguments don’t stand up against an analysis grounded in scientific evidence.
So this alleged overload on the immune system doesn’t really happen?
The overload has never been proven. Hypothetically speaking, if I administer 10,000 vaccines to one child at the same time, he has the ability to respond to all of them, without any overload. The argument about overload goes like this: when your body is vaccinated multiple times, your immune system is overloaded because it has to respond to the vaccines and can’t respond to other threats. This concept presupposes that humans, especially younger ones, are incapable of responding efficaciously and safely to the large number of antigens found in vaccines. But look: when a baby is born, within a few hours its intestines are completely populated by bacteria. The amount of antigens that it receives is thousands of times greater than the antigens given during vaccination. If there were an immune system overload, children would die in the first few days of life, because postnatal bacterial colonization would be enough to kill the baby.
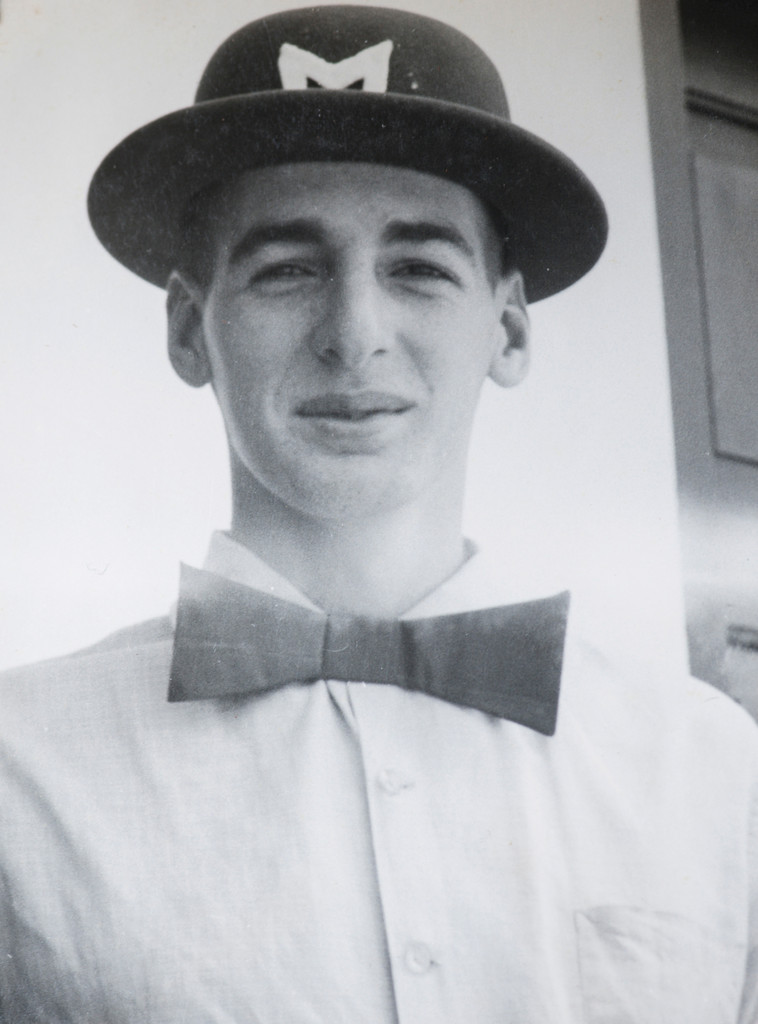
Personal archives In 1961, while at the Sorocaba School of MedicinePersonal archives
What prompted people to reject vaccines in the past?
In 1904, Rio de Janeiro witnessed the Vaccine Revolt, which was a time of popular unrest and protests. The main cause was the mandatory smallpox vaccination campaign launched by the Brazilian government and led by Oswaldo Cruz, a public health physician. Most people were poor and didn’t have information on how vaccines worked. So the rebellion wasn’t against the vaccine itself but against ordering people to be vaccinated. In the late 19th century, England decided to abolish mandatory vaccines. Instead of prompting a drop in the number of people vaccinated, the opposite happened: people voluntarily agreed to be vaccinated.
Is forcing people to be vaccinated still problematic?
Mandatory vaccination is an ethical, moral, and cultural issue. In the United States, 48 states allowed people to refuse to have their children vaccinated if they presented a religious or philosophical argument or for medical reasons. The two exceptions were West Virginia and Mississippi, where vaccination is mandatory. For children to enter school there, proof of vaccination must be shown. California recently began demanding basic vaccination as a requirement for school enrollment. Three years ago, Australia adopted a different strategy when they realized that population vaccination rates were dropping to dangerous levels. The solution was to offer financial rewards to parents who have their children vaccinated.
Brazil chose to recommend and offer vaccines instead of making them mandatory. In your opinion, is that the right thing to do?
We had a discussion about this within the Ministry of Health here in Brazil. In my opinion, in a country like ours, refusing to let a child enroll in school because his vaccines are not up to date is a very bad idea. Access to education is appalling here and there’s no reason to make it worse. In Australia, before they adopted the reward method, they let unvaccinated children attend school. But if there was an outbreak of a disease, that child could be suspended, whether the suspension were to last a month or a year. We have a lot of work left to do here using information. For instance, we could ask parents to enroll their children in school and present their vaccination cards. If the shots aren’t up to date, the parents could be called in and the importance of vaccination explained to them, and they’d be told about the public health clinics in the neighborhood where they could have their children vaccinated for free. That way, schools wouldn’t simply be refusing to admit a student but would be educating parents and giving them at least a minimum amount of information on how to proceed. If we do this, we can improve vaccination rates in Brazil. They’re good, and they can get better.
Are there any caveats about vaccines that actually have a scientific basis?
There have been some times in history when mistakes occurred during vaccine production – something quite rare today. For example, a contaminated batch of Sabin vaccine was distributed in the early 1960s. A series of steps are followed today, like checking for impurities and different phases of human testing. So it’s unlikely for there to be side effects that are unforeseen or weren’t verified during clinical trials. The steps in manufacturing a vaccine are similar to those for a drug, and it can take over 10 years for a vaccine to reach the market. Vaccines don’t have any really significant side effects. You might see a febrile seizure in a child once in a while, but it’s not common. Another example: when you get the pneumococcal vaccine for the first time, you start forming antibodies. When you get the second dose, if you have a lot of antibodies, you might have a local skin reaction and be achy for a few days. The trouble is that a lot of people get the vaccine and aren’t told about this side effect. The reaction scares them, they go to the emergency room, and there they end up being treated as if they had some kind of infection.

Personal archives
Guido Levy with then-governor Mário Covas at the re-inauguration of the intensive care unit of the Emílio Ribas Institute, in 2000Personal archivesWhat are your thoughts on research into dengue vaccines?
Clinics around the country should soon have a vaccine developed by the firm Sanofi Pasteur. But the efficacy rate for this vaccine isn’t very high – it protects about 60% of the time. Studies have shown that this particular vaccine is more efficacious in people who have already had dengue. It’s given in three doses with a six-month interval between one dose and another. If you were to have an outbreak in a certain place, it would be hard to stop it with a vaccine like this. Brazil’s National Immunization Program isn’t considering purchasing the vaccine at present. The fact is that research is being done on other dengue vaccines that seem to display greater efficacy. The Butantan Institute developed one of these, in conjunction with the National Institutes of Health – the largest medical research funding agency in the United States – and it has reached Phase III trials [from 2008 to 2011, FAPESP, in partnership with the National Council for Scientific and Technological Development (CNPq) and the Ministry of Health, funded initial work on this vaccine under the auspices of the Research Partnership for Technological Innovation Program (PITE)]. Bio-Manguinhos – the Institute of Technology in Immunobiologicals, which is an arm of the Oswaldo Cruz Foundation (Fiocruz), in Rio de Janeiro – is also processing a vaccine that promises to be effective in fighting dengue. In the coming years, we’ll have good vaccines against the disease.
The pharmaceutical industry doesn’t find vaccine production attractive. What can be done to guarantee that vaccines are developed and produced?
In the past, a rich country could afford to take little interest in producing a drug or vaccine for a given disease that is typical of developing nations. But now the world is globalized. People get around more and this makes it easier for viruses to spread. Dengue is no longer limited to countries in the southern hemisphere; cases have been reported in the United States, just as malaria and Ebola have been reported in Europe. All countries need to be prepared. That’s why recent years have witnessed an increase in partnerships between businesses, research institutions, and nongovernmental organizations as a way of accelerating the development of vaccines and drugs. But we still need more incentives for this type of collaboration.
What are your thoughts on vaccine production in Brazil?
The yellow fever vaccine is manufactured by Fiocruz and the flu vaccine by the Butantan Institute, although part of it is done at the Sanofi Pasteur laboratory. But overall, production is still in its infancy here. We’re not self-sufficient. One smart thing that’s being done are partnerships involving technology transfer. A Brazilian institution purchases the pneumococcal vaccine from an international laboratory, for instance, under the condition the lab transfer its technology. That way, five years down the road, Brazil can make the vaccine.
The vaccine against the HPV virus can help fight some types of cancer. Is there greater acceptance of the relationship between viruses and cancer today?
This hypothesis about the virus was important enough that Brazil’s federal government included the HPV vaccine – which is very expensive – on its national schedule. HPV has been associated with cases of pharyngeal, laryngeal, rectal, penile, anal, and cervical cancer. I think this outlook, associating cancer with viral causes, should be taken more seriously. We can say that the HPV vaccine works against cancer indirectly. Some people say there’s no evidence that this vaccine fights cancer. But of course there are a number of stages between being infected by the virus and developing a cancer. The idea is that the vaccine keeps these intermediary stages from developing. Twenty years from now, we’ll know for sure whether the vaccine helped avoid cases of cancer.
Girls from the age of nine on up are being vaccinated to prevent HPV contagion and re-infection. Shouldn’t boys be taken into consideration as well to make control more efficient?
This differentiated treatment is for economic reasons. Brazil has made a huge effort to promote the vaccine. The first stage of vaccination covered 100% of the target group. The focus has been on girls because cervical cancer is the most serious. In countries where money isn’t a problem, both genders are vaccinated, which is what happens in Australia today. In fact, I had both my granddaughters and grandsons vaccinated. I don’t care about statistics, which show that cervical cancer is more common than laryngeal. So what? All forms of cancer should be combated.
If Brazil has a public vaccine distribution network, what’s the point of having private clinics like CEDIPI?
The clinic offers vaccines that aren’t available through the public network yet. We purchased the MMR vaccine long before it was offered by the public network. We’ve been able to get some vaccines earlier by negotiating directly with laboratories. For example, the private network offers the meningitis B vaccine, which isn’t available through the public network, just as we offer the vaccine to prevent shingles, which also has yet to be included in Brazil’s Unified Health System (SUS). Furthermore, even though CEDIPI doesn’t conduct research, a good part of our staff works with research institutions and agencies like the State Department of Health and the Ministry of Health. Just because we are a private clinic, that doesn’t mean we’re going to stop fighting for more vaccines to be included in the public network. To the contrary.