An international collaboration involving researchers from the University of São Paulo (USP) and the Oswaldo Cruz Foundation (FIOCRUZ) in Rio de Janeiro identified two human antibodies with the potential to treat yellow fever, a disease that in its most severe form kills 20–50% of patients. Rodents and monkeys treated with the two molecules were able to survive infection with the virus that causes the hemorrhagic fever and damages the liver, kidneys, and to a lesser extent, the heart and lungs. The untreated control group became seriously ill and had to be euthanized about a week after being infected with the virus.
“To our surprise, the antibodies offered total protection against yellow fever,” says infectious disease specialist Esper Kallás of USP, one of the authors of the resulting paper published in the journal Science Translational Medicine in March. As the effects observed in other species do not always occur in people, human testing is still needed to confirm the results, but if everything goes as hoped, these antibodies could one day offer an effective therapy for yellow fever.
The search for an antibody-based treatment for the disease began about six years ago during the 2016–2019 outbreak, the most serious recorded in Brazil in the last eight decades, in which 2,237 people fell ill and 759 died. On a visit to USP’s Hospital das Clínicas, pathologist David Watkins of George Washington University in the USA, coauthor of the paper and a long-term partner of the Brazilian scientists, watched as people infected with the virus arrived at the health center feeling relatively well, but days later needed to be intubated and given hemodialysis to take over the role of their organs and bodily systems compromised by the disease. Watkins asked how he could help, and Kallás suggested that they try to develop a therapy based on synthetic versions of antibodies—the molecules naturally produced by the immune system to fight off invading organisms.
There is currently no specific treatment for yellow fever. When a person becomes seriously ill with the disease and needs to be hospitalized, their treatment consists of supportive measures to keep the body hydrated and prevent bleeding and kidney damage. The best protection against the disease is the vaccine, made with an attenuated (weakened) version of the virus. Developed nearly a century ago, it is effective and safe. Within a few weeks of immunization, it prevents almost 100% of recipients from developing the severe form of the disease. Although it is part of the vaccination program in around 40 countries where the infection is endemic—including Brazil—the proportion of people who get the vaccine is low. Data from the Pan American Health Organization (PAHO) indicate that on average, just 50% of people in these nations receive the vaccine, which can cause adverse events in rare cases. In approximately 1 of every 250,000 people vaccinated, the virus is able to multiply and goes on to cause the severe form of the disease.
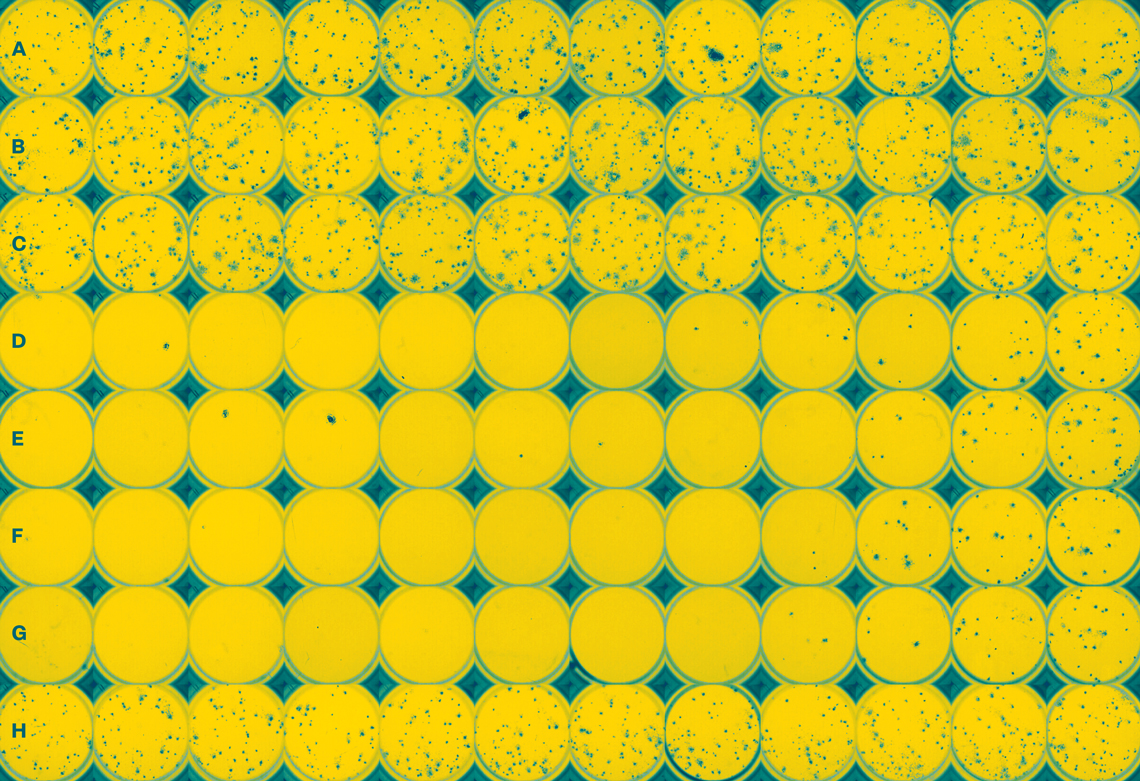
After returning to the USA, Watkins contacted immunologist Laura Walker, currently at Adagio Therapeutics, who had isolated around 1,200 different antibodies produced by the bodies of people vaccinated against yellow fever. Watkins’ team selected the 37 most promising antibodies and tested each of them in the lab to determine how well they stopped the virus. The five that performed best were sent to biologist Myrna Bonaldo in Rio de Janeiro. At FIOCRUZ, Bonaldo’s group tested their ability to neutralize four strains of the virus that circulated in Brazil between 2008 and 2019.
Two of the antibodies analyzed at FIOCRUZ (MBL-YFV-01 and MBL-YFV-02) proved to be particularly promising and were chosen to test on animals. Administered separately to hamsters in single doses three days after infection with the yellow fever virus, the antibodies reduced the severity of the disease. The animals all lived for the full 21 days that they were monitored. The hamsters in the control group began to die on the sixth day after infection. At Oregon Health and Science University, USA, biologist Benjamin Burwitz repeated the experiments with rhesus monkeys, in which the infection tends to be more aggressive, often causing death within three days, and obtained similar results.
“Due to their proven ability to neutralize the virus, these antibodies are ready for clinical trials,” says Kallás, director of the Butantan Institute. “In the future, it could be interesting to test the two antibodies in combination, because each one recognizes a different region of the virus envelope,” suggests Bonaldo, from FIOCRUZ.
Before human testing begins, however, a common problem in the development of medicines and vaccines in Brazil needs to be overcome: the production of antibodies in accordance with the good manufacturing practices required by health agencies for use in human beings. “It currently costs at least US$5 million to produce a pilot batch of these antibodies abroad,” reports the infectious disease specialist from USP.
“If they prove efficient in human trials, these antibodies could represent a major advance in the treatment of yellow fever,” says physician and virologist Pedro Vasconcelos, from the Evandro Chagas Institute (IEC) and the State University of Pará (UEPA) in Belém, who did not participate in the research. Part of the Flaviviridae family, which also includes the dengue and Zika viruses, yellow fever affects around 200,000 people worldwide every year and manifests itself in two stages. The first—the infectious phase—lasts three or four days and causes high fever, chills, fatigue, headaches, muscle pain, nausea, and vomiting. Then, in the viscerotropic phase, the virus attacks organs such as the kidneys, liver, heart, and lungs, causing damage that can be fatal. “Having monoclonal antibodies that prevent the disease from progressing from the infectious phase to the viscerotropic phase could increase survival of infected individuals and reduce the lethality of the disease,” says Vasconcelos. The researchers theorize that these antibodies could also be used to combat rare adverse events caused by the vaccine.
Project
Investigation of neutrophilia in patients with acute yellow fever (no. 19/13713-1); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Esper George Kallás (USP); Beneficiary Mateu Vailant Thomazella; Investment R$148,324.57.
Scientific articles
RICCIARDI, M. J. et al. Therapeutic neutralizing monoclonal antibody administration protects against lethal yellow fever virus infection. Science Translational Medicine. Mar. 29, 2023.
HASLWANTER, D. et al. Genotype-specific features reduce the susceptibility of South American yellow fever virus strains to vaccine-induced antibodies. Cell Host Microbe. Feb. 9, 2022.