In early June, psychiatrist and epidemiologist Cleusa Ferri of the Federal University of São Paulo (UNIFESP) was hard at work on an extensive and important report that she will present to Brazil’s Ministry of Health in September. Drafted together with experts in neurology, geriatrics, and mental health, the document contains the most recent estimates, calculated for the entire country for the first time, of a problem expected to hit the health system with full force in the coming decades: the increase in cases of dementia. Specialists hope the report will encourage the government to act and contribute to a national strategy addressing the issue, something that has been recommended by the Pan American Health Organization (PAHO) since 2015.
Time is of the essence. At least 1.76 million Brazilians over the age of 60 currently suffer from some form of dementia, a group of incurable illnesses that, through various mechanisms, cause the progressive loss of brain cells, ultimately leading to disability and death. Most of these people — an as yet unknown proportion that could exceed 70%, according to experts — have not even been diagnosed, which means they do not receive the treatment needed to control the changes in memory, reasoning, mood, and behavior that arise as the disease progresses.
Ferri and neuropsychologist Laiss Bertola arrived at this estimated percentage after carrying out neuropsychological and day-to-day functional competence tests to measure the number of people with dementia in a group of 5,249 individuals, a representative sample of the Brazilian population aged 60 or over. The researchers extrapolated their estimate (5.8%) to the rest of the Brazilian population of the same age group, based on the most recent national census, from 2010. The number was then adjusted to account for the increase in the number of elderly people in the years since. The results were originally published in the Journal of Gerontology on January 22.
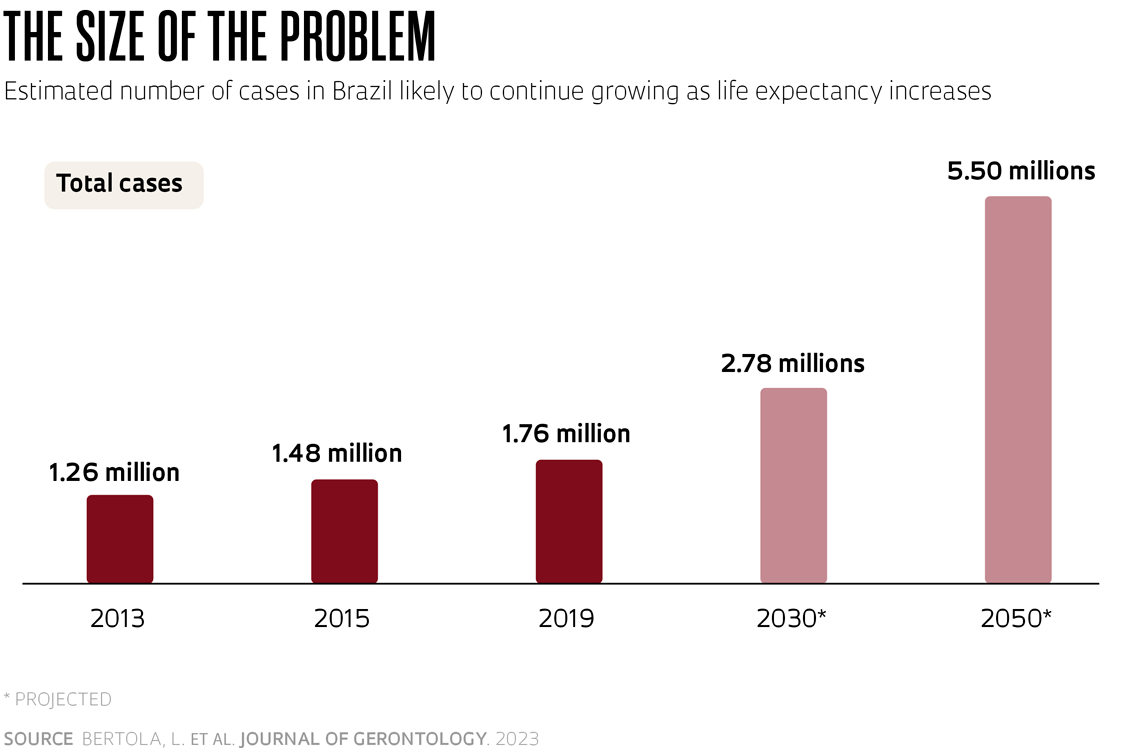
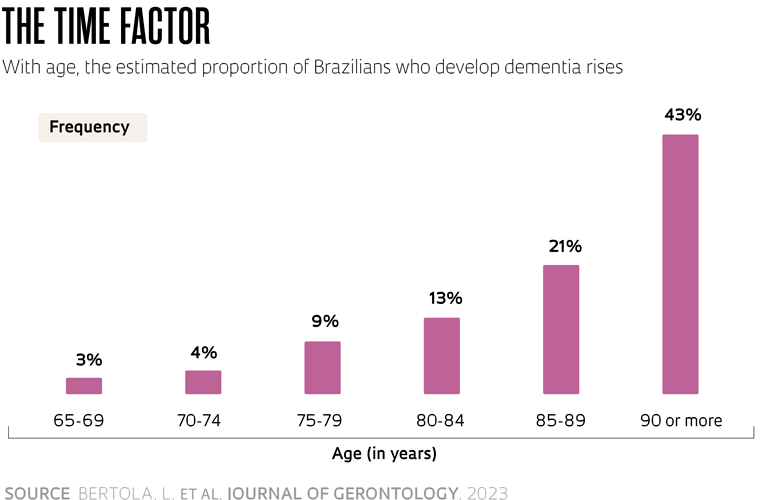
According to the article, the total number of cases in 2019 was about 20% higher than four years prior, when it was estimated that there were 1.48 million people with dementia in Brazil. And this figure is expected to grow, with projections that it will reach 2.78 million by the end of this decade and 5.5 million by 2050. The proportion of individuals with the disease increases significantly with age, although experts and the World Health Organization (WHO) state that it is not a characteristic of normal aging. Brazilian data indicate that 3% of individuals aged between 65 and 69 years develop dementia. This rises to 9% in the 75 to 79 age group, 21% in 85- to 89-year-olds, and 43% after the age of 90.
“This information is crucial for the country to prepare to address the situation and create the services required to meet the needs of these people,” said Ferri, who in June was still trying to complete her calculations of how long it takes for each new case to arise among Brazilians, on average. “The document recommends that the Ministry of Health and other agencies monitor the number of cases over time. It also suggests what steps need to be taken to reduce people’s risk of developing dementia,” says the researcher, whose father died 15 years ago with one of the forms of the disease.
The rising number of dementia cases is not exclusive to Brazil. In much of the world, improvements in living conditions achieved over the last century have allowed people to live longer. In 2005, there were around 670 million people aged 60 or over worldwide, equivalent to 10% of the global population. In 2050, according to projections by the United Nations (UN), there will be almost 2 billion — equal to 22% of humanity.
With the world’s population growing and life expectancy increasing, more cases of dementia are expected. In a February 2022 article in the journal The Lancet Public Health, an international team of researchers estimated that 57.4 million people worldwide were living with some form of dementia in 2019. This number, according to their calculations, will grow by 2.7 times by the middle of this century, reaching 152.8 million.
It is a huge problem that will not affect all countries uniformly and will soon need to be tackled. Cases are expected to increase at a greater rate in low- and middle-income countries — in Latin America they will triple — which will overload healthcare systems and families alike. Dementia is one of the biggest causes of disability in the elderly and has a physical, psychological, social, and economic impact both on the people with the disease and on those who care for them. According to the WHO, US$1.3 trillion was spent on caring for people with dementia globally in 2019.
“There are three factors behind the greater increase in these countries,” says Paulo Caramelli, a neurologist from the Federal University of Minas Gerais (UFMG) and coauthor of a recent study on dementia in Latin America. The first is that the populations of low- and middle-income countries are aging very quickly. It took almost 150 years for the proportion of elderly people to rise from 10% to 20% of the population in France, one of the nations with the oldest populations in the world, while in countries like Brazil, this transition is going to occur in just over two decades. The other two reasons are improvements in diagnosing dementia and poorer management of health problems — especially diabetes, hypertension, and obesity — that contribute to the disease’s development. “In the USA and Europe, where the population has already reached the life expectancy ceiling and the risk factors are better controlled, the prevalence will decrease in the coming decades,” says the researcher, who specializes in dementia.
 Belisa Bagiani
Belisa Bagiani
Alienation, foolishness, and senility
Possibly as old as humanity itself, dementia — or some of the symptoms that characterize it — has been given many names throughout history. Alienation, amentia, stupidity, idiocy, imbecility, foolishness, and senility are just some of the terms listed by neurologists François Boller and Margaret M. Forbes in an article published in the Journal of the Neurological Sciences in 1998.
The derogatory connotation of some of these terms hints at how people with dementia have been treated for a long time. Often considered a nuisance, people who showed signs of delirium and agitation were confined in asylums or prisons before the emergence of psychiatric hospitals. Even in medical institutions, they were frequently kept in chains, deprived of food and clothing, or subjected to beatings, wrote American psychiatrist Tia Powell of the Albert Einstein College of Medicine in New York, USA, whose mother and grandmother both had the disease, in a chapter of the book Dementia Reimagined: Building a Life of Joy and Dignity from Beginning to End (2020). Things only started to change at the end of the nineteenth century, when some areas of medicine began seeing people with dementia from a more compassionate perspective.
What doctors call dementia today is a broad set of illnesses that can manifest at any time in life, but most often emerge after the age of 60 and inevitably lead to progressive deterioration of a person’s intellectual capacity.
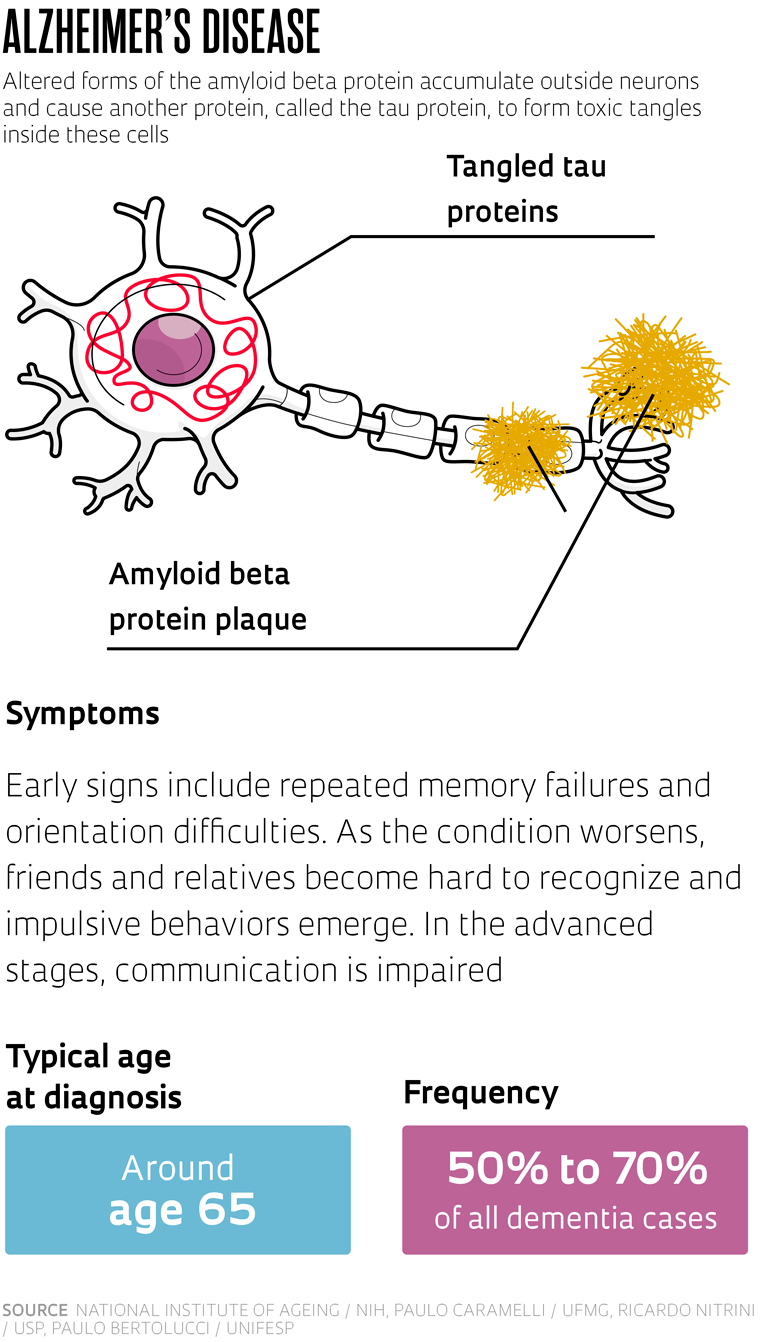
The most well-known and common is Alzheimer’s disease. Described in 1906 by German psychiatrist and neuropathologist Alois Alzheimer (1864–1915) and almost simultaneously by his Czech counterpart Oskar Fischer (1876–1942), the disease represents up to 70% of cases of dementia in high-income countries, and somewhere between 50% and 60% in Brazil, according to studies carried out in the country. The earliest sign, which is usually short-term memory problems, appears more frequently after the age of 65.
Two other forms of dementia, each accounting for less than 5% of all cases, tend to present earlier: frontotemporal dementia and dementia with Lewy bodies (DLB). The former is named after the fact that the lesions are concentrated in the anterior and lateral areas of the brain — the frontal and temporal lobes respectively — and affect the individual’s ability to plan, concentrate, and control impulsive behavior. Symptoms can begin to show from around the age of 45, slightly earlier than dementia with Lewy bodies, which is marked by problems with concentration, logical reasoning, and movement control and results from a type of lesion identified by German neurologist Fritz Henrich Lewy (1885–1950) in 1912.
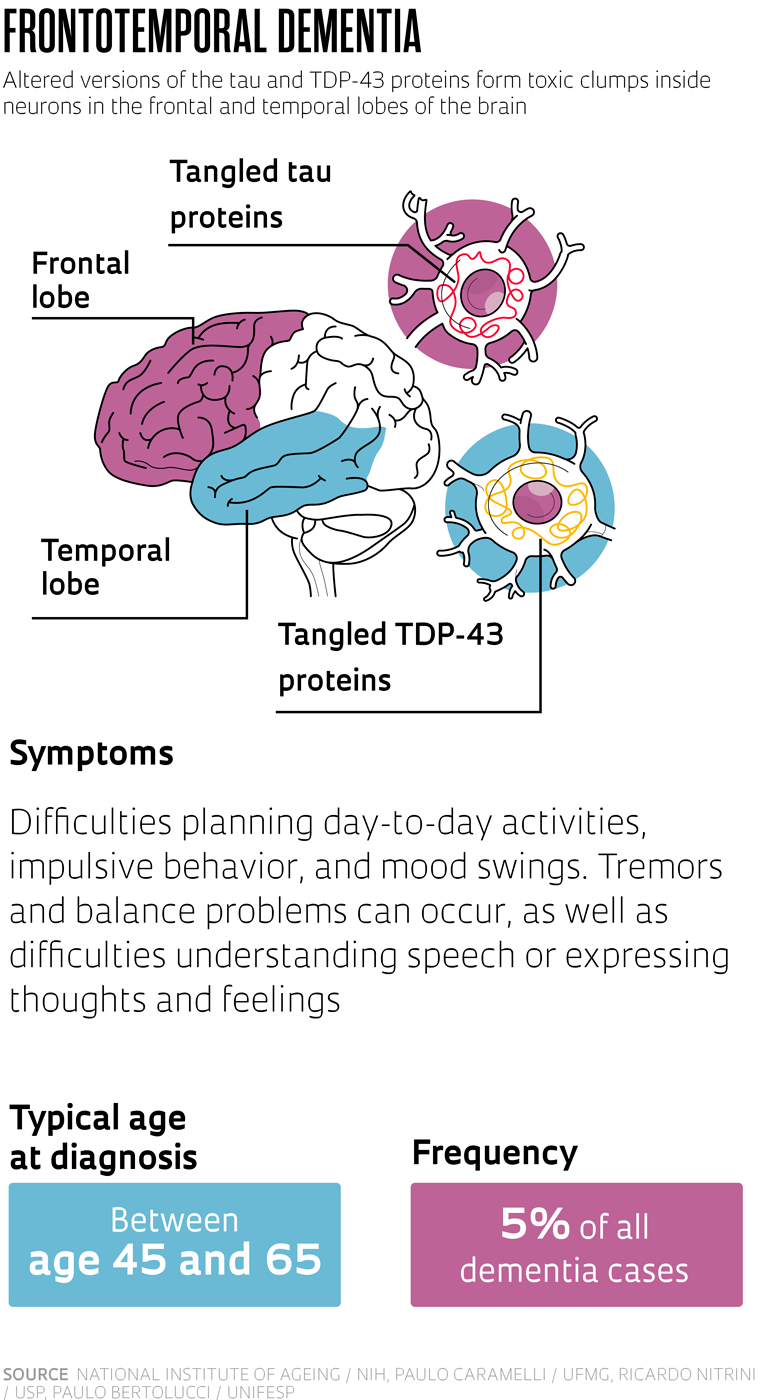
There is a common thread between the three. According to the most accepted current hypotheses, they all seem to be caused by an accumulation of deformed proteins in the brain. What changes from one to the other is the protein involved and the location of the deposits.
So far, none of the diseases have a cure. The drugs most used in the initial stages are acetylcholinesterase inhibitors. These compounds, such as donepezil, galantamine and rivastigmine, alleviate memory loss and difficulties in learning new functions by increasing availability of the neurotransmitter acetylcholine in the brain, which is important for cognition. Another treatment option generally used in the more advanced stages is memantine, which modulates the levels of another neurotransmitter called glutamate. In high concentrations, glutamate is toxic to neurons, the cells that function as information-processing units in the brain.

In the last two years, two new monoclonal antibodies have been launched that slow the progression of Alzheimer’s: aducanumab and lecanemab. Aducanumab, developed by American biotechnology company Biogen, was approved by the US Food and Drug Administration (FDA) in 2021 and is sold in the USA under the brand name Aduhelm. Lecanemab, manufactured by Japanese pharmaceutical company Eisai, was authorized by the FDA this year and is branded as Leqembi. Both are designed to eliminate clusters of amyloid beta, a protein typical of Alzheimer’s. These drugs, however, are expensive. The annual cost of treatment exceeds US$25,000 per patient and the results are modest: the pace of cognitive decline is only moderately reduced, meaning the disease continues to progress, just at a slightly slower rate.
One possible explanation for the disappointing results is that the tests were carried out on people in intermediate stages of the disease, when protein plaque levels are already high. “In this phase, there are very large accumulations that are more difficult to break apart,” says Sérgio Teixeira Ferreira, a biochemist from the Federal University of Rio de Janeiro (UFRJ) who studies the causes of Alzheimer’s. Thus, current studies are examining individuals with the disease in earlier stages. But expectations remain conservative. “Neither studies with animals nor with human beings have offered any evidence that reducing the amount of plaques improves cognitive capacity and quality of life for people with the disease. Perhaps the most appropriate target would be the soluble — and toxic — forms, known as amyloid beta oligomers,” says the biochemist.
If there is no cure for these forms of the disease, is it even worth pursuing a diagnosis? The answer given by experts is yes. “There are some rarer forms of dementia that are reversible, such as those caused by thyroid gland disorders or vitamin B12 deficiency. Once the cause is treated, the problem disappears,” explains Caramelli.
What can be done
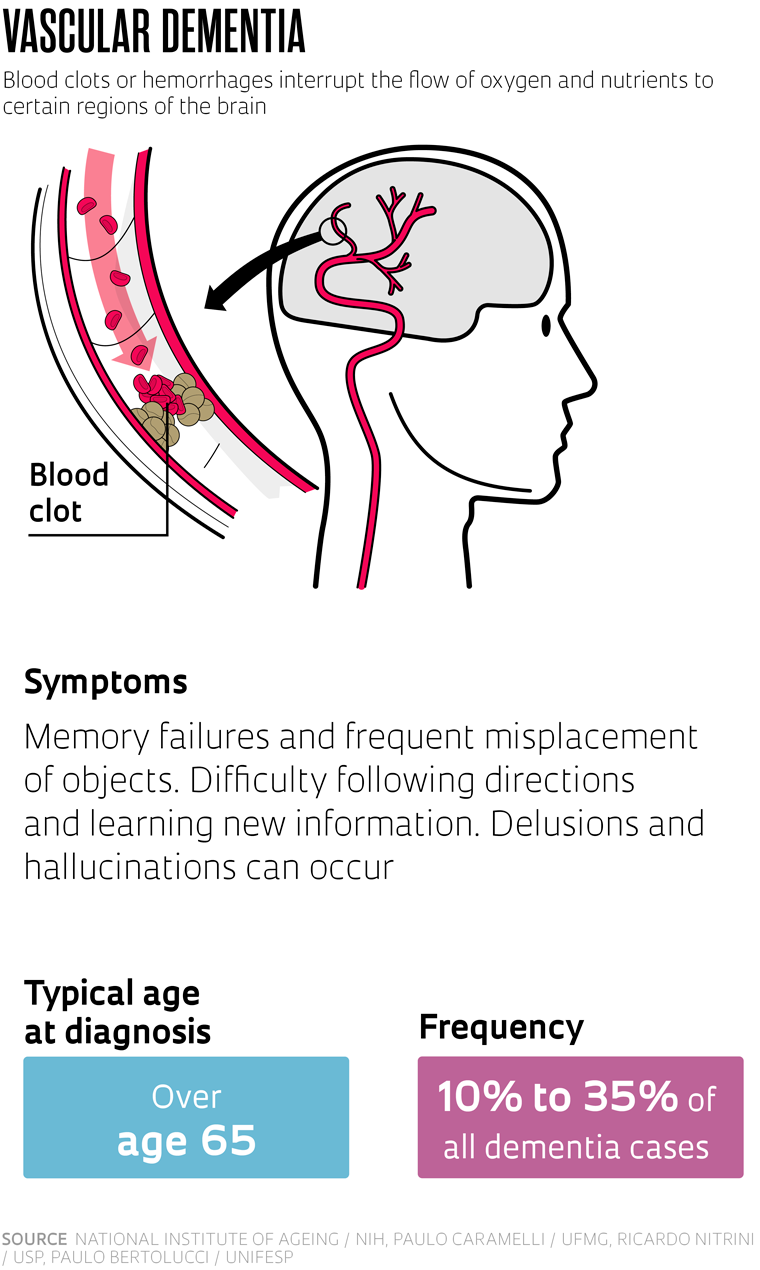
While there is not yet a cure for the most common types of dementia, and maybe there never will be, much can be done at the individual and public health level. The second most common form of the disease in many countries is vascular dementia. Caused by the blockage or rupture of the delicate blood vessels that irrigate the brain, leading to rapid cell death, it accounts for up to 35% of dementia cases in Brazil. The most important thing is that it can be prevented. “Vascular dementia is very preventable by properly treating the problems that affect the health of the vascular system, such as diabetes, hypertension, and obesity,” says Claudia Suemoto, a geriatrician from the University of São Paulo (USP).
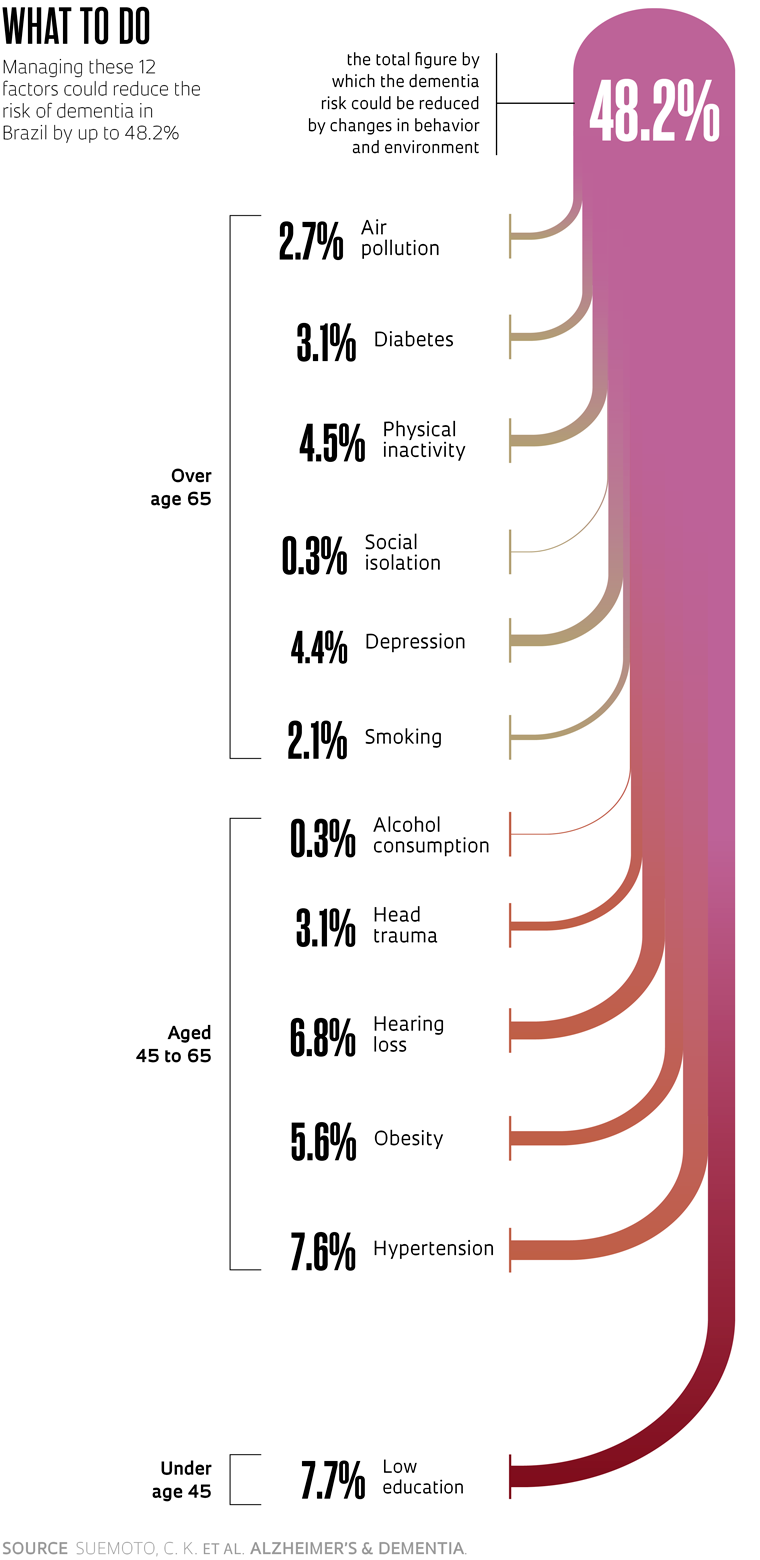
British psychiatrist Gill Livingston, a specialist in mental health of the elderly at University College London, has headed The Lancet’s commission on dementia prevention, intervention, and care for several years. In two lengthy reports, one published in 2017 and the other in 2020, the commission listed 12 factors associated with the risk of developing dementia that can be managed throughout life. They include low education, obesity, diabetes, hypertension, alcohol consumption, and physical inactivity, all of which have a recognized influence on brain health. Each factor was given a distinct weighting, calculated based on the strength of its association with the disease, its prevalence in the population, and its individual impact on dementia. If all were well managed, it would theoretically be possible to prevent or delay the onset of up to 40% of dementia cases. “It is now known that many of dementia’s manifestations are manageable and while the underlying illnesses are generally not curable, they may be modifiable with good care,” the authors wrote in the 2017 paper.
 Belisa Bagiani
Belisa Bagiani
The effects estimated by the international commission, however, were based on health information from the populations of rich countries. In Brazil, the potential for prevention is even greater.
In partnership with Livingston and researchers from Minas Gerais and Rio de Janeiro, USP’s Suemoto and UNIFESP’s Ferri recalculated the impact that managing these 12 factors could have in Brazil. If it were possible to eliminate them completely, cases of dementia would fall by 48.2%. They would decrease by up to 54% in the poorest regions of the country according to the data, which were published in Alzheimer’s & Dementia in November 2022 and will be included in the dossier to be presented to the Ministry of Health.
“Dementia is already a public health problem in Brazil. To reduce its impact in the future, we need to invest in policies that help reduce risk factors, especially those in early life and middle age,” says Suemoto. “If action is not taken, we are going to see a tsunami of cases, because the population is living longer,” warns USP neurologist Ricardo Nitrini, coauthor of the Alzheimer’s & Dementia article and a pioneer in studies of the epidemiology of dementia in Brazil.
The result will not be immediate, so the country must act as soon as possible. “The problem is highly imminent and any measures to alleviate it will only take effect in the medium and long term,” emphasizes Paulo Mattos, a retired professor of psychiatry at UFRJ and head of Neurosciences at the D’Or Institute for Research and Teaching, which investigates the biological causes of Alzheimer’s. “Changing these risk factors would take decades to have an impact at the populational level. Even at an individual level, the cognitive improvements provided by measures such as managing cholesterol levels and diabetes and performing regular physical exercise would take years to become evident,” he explains.
In Brazil, more so than in the rest of the world, the factor with the greatest potential for reducing dementia rates is educational level, especially in the poorest regions. The country only achieved universal access to primary education in the late 1990s, but according to 2019 data from the Brazilian Institute of Geography and Statistics (IBGE), less than half of people aged below 25 finish secondary education. If it were possible to eliminate the low educational level factor by ensuring nobody had less than eight years of formal education, 7.7% of dementia cases could be prevented. Among the poorest population, the reduction would be 9.6%.
Increasing educational levels and physical activity and managing obesity, diabetes, and hypertension can reduce the risk of dementia
Studies done in Brazil and abroad suggest that literacy and other activities learned at school promote anatomical and functional changes in the brain, stimulating the creation of connections between neurons and increasing the density of the fibers that transfer information between different regions of the brain. Neuroscientist Yakov Stern of Columbia University, USA, dubbed this increased connectivity in the brain “cognitive reserve.” The theory explains why some people show no signs of dementia despite having large amounts of protein plaques. An individual with high cognitive reserve has multiple brain networks and other compensatory mechanisms that allow them to circumvent the effects of the disease for a longer time, often only showing symptoms in the more advanced stages.
In Brazil, the type of impact provided by increasing educational level could also be achieved by better treating hearing loss, managing hypertension, and reducing obesity. “Improving education alone is not enough,” says Nitrini. “We need to encourage physical activity and a healthy diet. Many of these precautions need to be taken during pregnancy and in the earliest years of a child’s life, helping the brain develop a good cognitive reserve to overcome the adversities it will face during the person’s lifetime,” advises the neurologist, who founded USP’s Cognitive and Behavioral Neurology Group (GNCC).