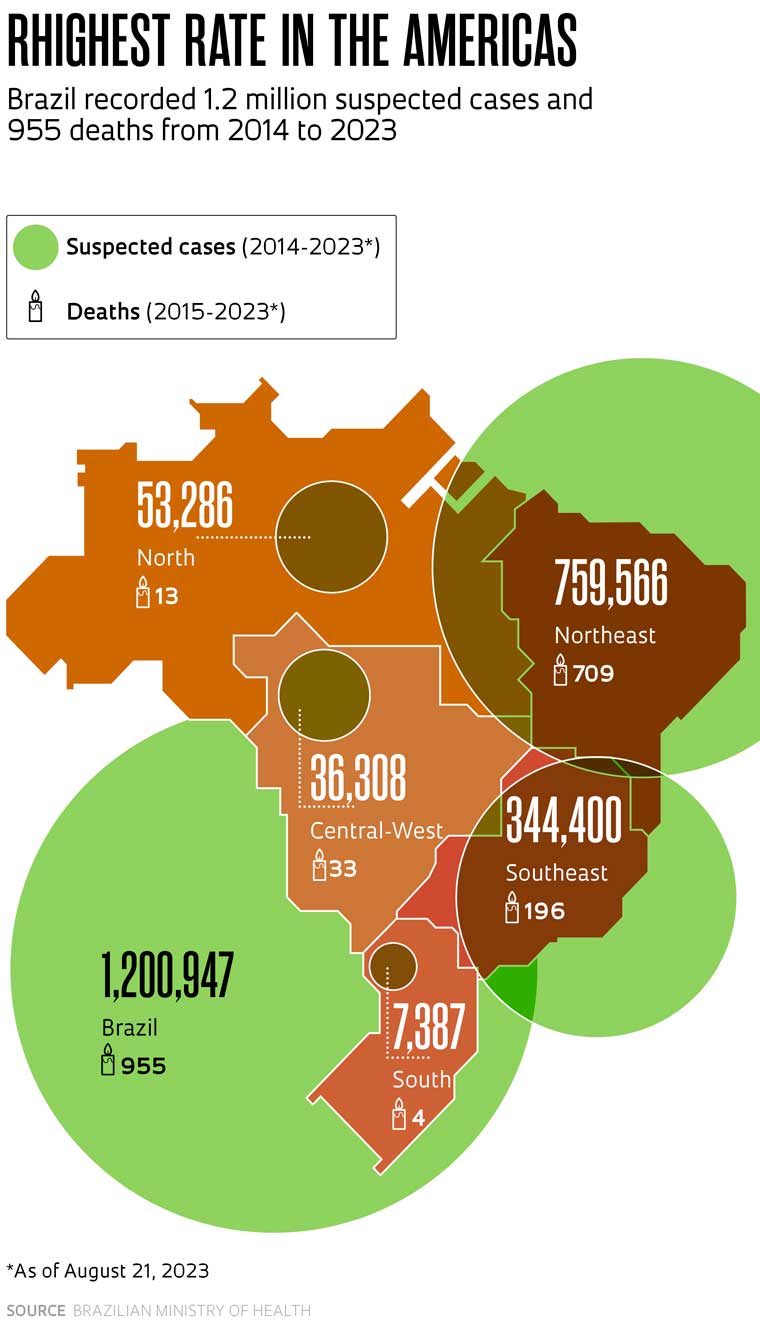
It appears the chikungunya fever virus has arrived in Brazil to stay, making it the country with the highest number of cases in the Americas. After the first case was identified in Brazil in 2014, the virus quickly spread across every state and has not stopped creating problems since. Over the past ten years, there have been at least seven major outbreaks—one per year since 2016—leading to almost 254,000 lab-confirmed infections and 1.2 million suspected cases, in addition to an estimated 1000 deaths. Two recent studies are helping scientists better understand the disease’s infection pattern and how the virus circulates, as it has accumulated genetic mutations capable of increasing its ability to replicate in a human host.
In the first study, published in April in the journal The Lancet Microbe, Brazilian virologist William Marciel de Souza from the University of Texas, in the United States, and collaborators in Brazil and abroad analyzed data from the 253,545 cases of chikungunya recorded across 3,316 Brazilian municipalities from March 2013 to June 2022. All cases were confirmed through laboratory testing to eliminate the possibility they were caused by dengue infection, which produces some symptoms similar to chikungunya. By evaluating the distribution of cases over time, the researchers identified seven major waves of infection (outbreaks). The peaks for each wave occurred between February and June, the hottest and rainiest months of the year in large parts of Brazil, conditions that favor the multiplication of virus vectors. The virus is transmitted to humans through bites from female mosquitoes of the species Aedes aegypti and Aedes albopictus, which are found in virtually every region of the country.
Next, Souza and his collaborators compared temporal information from the cases with their geographic distribution and identified a new pattern. Locations hit by an outbreak in any given year were spared in subsequent years. This pattern of occurrence gives credence to the idea that infection with the chikungunya virus leads to the development of long-lasting immunity, something previously suggested by studies with laboratory animals and tests with blood from people from other countries where the virus circulates. If this form of immunity actually occurs, an individual who is cured of the infection would be protected for years—possibly even for life—from further infection by the virus or at least from the possibility of developing the disease.
The patterns the group found also indicate that the virus spreads in small pockets, generally restricted to a few municipalities, which makes it possible that new outbreaks can occur in previously affected states. This became clear when data from Tocantins, Pernambuco, and Ceará were analyzed, states that have seen repeated outbreaks every few years. In these states, locations that experienced a high number of cases during one wave had a lower number in the next, indicating the dispersion of cases in pockets, while in areas where outbreaks had already occurred, there existed varying levels of immunological protection against the disease or its transmission. This proved true even in Ceará, where 30% of all Brazilian cases have occurred.
“In the first two epidemiological waves, the virus circulated a lot in the north of Ceará; in the last one, it hit municipalities in the southern part of the state,” says virologist José Luiz Proença Módena, from the University of Campinas (UNICAMP), one of the study coordinators. Modena worked with Ester Sabino, a physician from the University of São Paulo (USP), Portuguese biomedical scientist Nuno Faria, from Imperial College, in London, and American immunologist Scott Weaver, from the University of Texas. The study was funded by FAPESP, the National Council for Scientific and Technological Development (CNPq), and other international sources.
If, on the one hand, the populations of municipalities with greater circulation apparently become protected, on the other, those less exposed remain susceptible to infection. This makes a large part of the country fertile ground for the spread of the virus since outbreaks of chikungunya have not yet occurred in 40% of Brazilian municipalities, including the densely populated areas of the Southeast region. “Although we’ve identified a certain pattern of occurrence in the cases, we’re still unable to predict where the next outbreak will occur,” says Módena, of UNICAMP.
By closely investigating data from Ceará, where there have been 77,418 recorded cases since 2013, researchers also noted that the virus more frequently infected adult women, as well as children and elderly people of both sexes. These characteristics suggest that transmission occurs in the domestic environment, since these are people, in general, who spend more time at home. Another data point that emerged from this analysis was the mortality rate. The Ceará data showed that the chikungunya virus has caused death in 1.3 of every 1000 cases, a rate similar to that of dengue (1.1 deaths per thousand). “Although there is no reinfection as with dengue, chikungunya is also deadly,” says Souza, one of the study’s lead authors.
The second article, published in July in the journal Nature Communications and funded by the National Institutes of Health in the United States, helps complete the picture of chikungunya fever in Brazil by revealing certain genetic characteristics of the virus currently circulating. In their study, teams from more than 30 Brazilian institutions sequenced the genome of 422 samples of the virus obtained from people infected in 2021 and 2022, when there were 312,000 suspected cases in the country, and compared the data with that of another 1,565 genomes from previous outbreaks both in Brazil and abroad.
All recent domestic cases were caused by the virus of the East-Central-South African (ECSA) lineage, which is associated with death, both in people with poor health due to other diseases and in healthy individuals. The ECSA variant arrived in Brazil, more specifically in Bahia, around 2014. During this same period, a second variety was identified in Amapá, of Asian origin, as indicated in a study by researchers from the Evandro Chagas Institute (IEC), in Pará, published in 2015 in the journal BMC Medicine. As it replicated and infected insects and humans, the ECSA-lineage virus slowly accumulated changes to its genome (mutations) that have allowed it to be classified into two subgroups: Clade I, spread across the Northeast, Central-West, Southeast, and South regions of the country, and Clade II, found mainly in the Northeast.
Although the ECSA variant entered the country in the Northeast, the varieties in circulation today are derived from viruses that emerged in the Southeast region—probably in Rio de Janeiro—in early 2018 and were later reintroduced in the Northeast through human travel between the two regions. From there, the ECSA lineage spread to other regions of the country and into Paraguay.
Cynthia Goldsmith / CDC
Copies of the chikungunya virus as viewed with an electron microscope. The virus causes inflammation and severe joint painCynthia Goldsmith / CDCSome of the mutations have drawn researchers’ attention because they suggest that the virus may be adapting to their vectors’ organisms, and because of their ability to escape the immune system’s first line of defense—something that still needs to be confirmed by laboratory experiments. “We saw genetic changes that, in other viruses, have already been associated with increased capacity for replication and adaptation to the host,” says virologist Luiz Alcântara. A researcher at the René Rachou Institute, an Oswaldo Cruz Foundation (FIOCRUZ) research unit in Minas Gerais, Alcântara is one of the lead authors of the Nature Communications study, with virologist Marta Giovanetti and biologist Joilson Xavier.
“Both studies suggest that the virus is increasingly adapted to the conditions found in Brazil, which could lead to larger outbreaks,” comments virologist Maurício Nogueira, from the São José do Rio Preto School of Medicine (FAMERP), who did not participate in the research. “This could become a serious problem in the Southeast, the country’s most populous region, where the number of cases so far has been small, and the population remains susceptible to the virus.”
Recent 2023 data from the Brazilian Ministry of Health indicate that an eighth wave of chikungunya appears to be underway. As of the end of August, 142,500 possible cases of infection had been recorded across the country, 60% of them in Minas Gerais State, which had not yet seen a major outbreak. In São Paulo, the number of cases is still low at approximately 3000, however, the total number of deaths is at 12, almost double the number recorded in 2021 when there were 18,600 probable cases.
What is already worrying today could become worse as a result of climate change. Studies suggest that the increase in the planet’s average temperature could create ideal conditions for mosquitoes to transmit the chikungunya virus for more months of the year and in areas where the climate was previously unfavorable. “As there are no measures to control the mosquito, what halts transmission is winter, which in the North and Northeast is very mild,” comments virologist Pedro Vasconcelos, from the IEC.
First identified in 1952 in Tanzania, infection with the “chikungunya” virus—an expression from the Kimakonde language meaning “that which bends up”—causes high fever and intense pain and swelling in the joints, in addition to symptoms similar to those of dengue and Zika, such as fever and rash. To date, there is no specific medication to combat the virus, and treatment consists of administering medication to reduce fever and relieve pain.
There is a promising vaccine, currently in the final phase of testing in humans, which could be available within the next few years. Developed by the French biotech firm Valneva, the potential vaccine, known only by the acronym VLA 1533, uses a live attenuated virus to stimulate an immune system response. Initial results from a Phase 3 clinical trial, published in June this year in The Lancet, indicate that the compound is safe and immunogenic. Administration of a single dose was enough to generate neutralizing antibodies in 98% of people. In Brazil, the Butantan Institute is currently evaluating the effectiveness of the VLA 1533 vaccine in 750 adolescents from 9 states. For now, however, the most efficient way to prevent outbreaks is to combat the mosquitoes.
Project
The UK-Brazil Joint Center for Arbovirus Discovery, Diagnosis, Genomics, and Epidemiology (CADDE) (nº 18/14389-0); Grant Mechanism Thematic Project; Principal Investigator Ester Cerdeira Sabino (USP); Investment R$9,281,439.23
Scientific articles
DE SOUZA, W. M. et al. Spatiotemporal dynamics and recurrence of chikungunya virus in Brazil: An epidemiological study. The Lancet Microbe. May 2023.
XAVIER, J. et al. Increased interregional virus exchange and nucleotide diversity outline the expansion of chikungunya virus in Brazil. Nature Communications. July 21, 2023.
TEIXEIRA NUNES, M. R. et al. Emergence and potential for spread of chikungunya virus in Brazil. BMC Medicine. Apr. 30, 2015.
SCHNEIDER, M. et al. Safety and immunogenicity of a single-shot live-attenuated chikungunya vaccine: A double-blind, multicentre, randomised, placebo-controlled, phase 3 trial. The Lancet. June 24, 2023.


