 Léo Ramos ChavesIn 2009, Brazilian epidemiologist Eduardo Franco joined in a public debate about the need to vaccinate girls against the human papilloma virus (HPV), the culprit behind cervical cancer – notably girls attending Catholic schools in the city of Calgary, Alberta Province, Canada (the matter prompted no discussion in Protestant schools). One year earlier, the local bishop had handed down an ecclesiastical decree banning HPV vaccination on the grounds that it would encourage sexual promiscuity. Franco decided to enter the fray after a colleague urged him to defend his arguments in public, rather than limiting his ideas and research to scientific papers. Under pressure from scientists, public health agency staff, and the parents of students, the bishop eventually withdrew the ban. Two years later, Franco spoke out against Brazil’s prevention strategies. In January 2017, Brazil added the HPV vaccine to its national vaccination schedule, for the first time extending it to boys ages 12 to 13.
Léo Ramos ChavesIn 2009, Brazilian epidemiologist Eduardo Franco joined in a public debate about the need to vaccinate girls against the human papilloma virus (HPV), the culprit behind cervical cancer – notably girls attending Catholic schools in the city of Calgary, Alberta Province, Canada (the matter prompted no discussion in Protestant schools). One year earlier, the local bishop had handed down an ecclesiastical decree banning HPV vaccination on the grounds that it would encourage sexual promiscuity. Franco decided to enter the fray after a colleague urged him to defend his arguments in public, rather than limiting his ideas and research to scientific papers. Under pressure from scientists, public health agency staff, and the parents of students, the bishop eventually withdrew the ban. Two years later, Franco spoke out against Brazil’s prevention strategies. In January 2017, Brazil added the HPV vaccine to its national vaccination schedule, for the first time extending it to boys ages 12 to 13.
In collaboration with Luisa Villa, who was then with the Ludwig Institute for Cancer Research and is now with the São Paulo State Cancer Institute (ICESP), Franco conducted a 10-year, pioneer study of 2,528 women in São Paulo that demonstrated a clear association between persistent HPV infection and cervical cancer. The research project, which ran from 1980 to 1990, has produced 46 published papers since 1999. One of the latest articles, published in BMC Infectious Diseases in March 2016, shows that cervical inflammation might increase the risk of HPV infection.
Franco is chairman of the Department of Oncology and director of the Division of Cancer Epidemiology at McGill University, in Montreal, where he has resided since 1989. He was in São Paulo in November 2016 for a meeting of the A.C.Camargo Cancer Center science advisory board, at which time he gave the first part of this interview, later continued via Skype.
In the interview, Franco, who has four children and three grandchildren from his three marriages, recalls people who he considers examples of civic and social engagement, leadership, and generosity who played important roles in his education, like physicians Ricardo Brentani (1937-2011; see Pesquisa FAPESP Issue nº 190); Sidney Arcifa (1938-2015); Antonio Carlos Corsini (1946-1984); and Humberto Torloni (1924-; see Pesquisa FAPESP Issue nº 216). He also talks about his current research, including investigations of a gel made from carrageenan, a polysaccharide extracted from algae. If the gel works as hoped, it may offer a low-cost, broad-spectrum strategy for fighting the HPV infections that can lead to cervical cancer.
| Age |
| 63 |
| Specialty |
| Epidemiology and cancer prevention |
| Education |
| Undergraduate degree in biology from the University of Campinas (Unicamp), 1975, and master’s and PhD from the University of North Carolina at Chapel Hill, 1981-1984 |
| Institution |
| McGill University, Montreal, Canada |
| Scientific production |
| 441 articles, H-index: 71 2 books on the epidemiology of cancer, 59 book chapters, and 73 graduate students and 28 postdoctoral fellows supervised |
How did you go from scientist closed inside the world of science to activist in the prevention of cervical cancer?
I always tell my students that science alone can’t change anything. We have to advocate and defend our work to healthcare administrators if we really want to change anything. But for many years, I believed that a scientist’s work should be separate from the role of promoting results, which would fall to other people. I thought I’d be renouncing my scientific integrity if I were to defend my own work. It was Juliet Guichon, a colleague of mine and bioethicist at the University of Calgary, who changed my view of the scientist’s role, in 2009. She asked for help because Frederick Henry, Bishop of the Diocese of Calgary, in Alberta Province, and leader of the Board of Trustees of the Calgary Catholic School District, had handed down a decree prohibiting public health nurses from vaccinating Catholic school girls against HPV.
Why?
Henry, as the bishop who wielded authority over Catholic schools, alleged that the HPV vaccine would cause promiscuity and that the best way to avoid contracting an HPV infection would be simply to abstain from sex before marriage. I gave Juliet some advice, but I didn’t work with her. One day, over the phone, she bawled me out: “Quit teaching me and do a little! You’ve got to stand up to the bullies with me!”
What did you do?
I wrote an article with her and Ian Mitchell, also from the University of Calgary, which was published in the Calgary Herald, and I went on a radio program with the bishop. He was in the studio but, owing to other commitments, I spoke by phone from a hotel in Banff, about 100 kilometers from Calgary. I argued that if the bishop prohibited the girls from receiving the vaccine, some might develop cervical cancer 20 years down the road. If they knew the vaccination ban had caused their disease, they could sue the bishop’s successors. He got really annoyed and said the province of Quebec, where I live, shouldn’t meddle in Calgary’s affairs. Then I asked Juliet to write a paper for the magazine Preventive Medicine, of which I’m editor. She also went out to the schools and talked with parents, who were persuaded that the bishop was only a church authority and had nothing to do with public health. Juliet and other researchers from the University of Calgary also sponsored public debates, drafted a letter – signed by more than 50 doctors – and sent it to the bishop’s board, and published articles in newspapers, which ultimately also called for the ban to be lifted. Given all this pressure, the bishop revoked the ban, and vaccination was evenly balanced at Protestant and Catholic schools.
What were your criticisms of Brazil?
During a conference in Rio de Janeiro, in 2011, I argued that the Ministry of Health’s policy for fighting cervical cancer was completely wrong. The ministry alleged that it wasn’t going to adopt HPV vaccination because it’s so costly. This premise was false, because the government wouldn’t have to pay private prices for the vaccine if it relied on centralized purchasing. The ministry also said there was no evidence that this prevention strategy might be efficient. In point of fact, there had been no multi-country clinical trial long enough to prove a reduction, because cervical cancer takes 20 years to start appearing, but they did show that the vaccine prevents both the infection and precancerous lesions. The government later altered its strategy and adopted HPV vaccination. The initiative got off to a good start, with the first campaign reaching more than 90% of girls with the first dose, because vaccination took place at school. Then they decided to give the second dose at public health clinics – I imagine to lower costs – and coverage dropped sharply.
What’s prevention like in Canada?
Vaccination began in 2007, shortly after the vaccine was approved. The health team in Quebec Province adopted the strategy of vaccinating younger, pre-adolescent girls, ages 9 to 10, rather than adolescents, in the belief that they could provide the same protection with two doses instead of three, and it worked. Most of the provinces also adopted vaccination for boys, using the same school vaccination policy, which ensures a high rate of coverage – 80% or more – with two doses.
In 2011, you also criticized Brazil’s public health system for continuing to use the Pap smear, a cytological screening method, to detect new cases of cervical cancer. Why?
As much as the Pap smear was an undeniable boon for humanity, it’s obsolete today and not very accurate compared to molecular methods like PCR [polymerase chain reaction], which identifies the virus’s DNA. The Pap smear yields a high number of false negatives. Precisely because there are so many false negatives, women have to repeat the test every year to increase their chances of catching a lesion indicative of cervical cancer. With PCR, the test doesn’t need to be done every year.
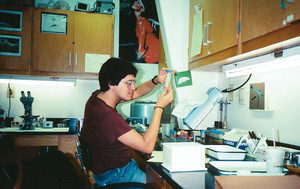
Personal archives
Franco at the CDC laboratory in Atlanta in 1983Personal archivesWhy did you study biology as an undergraduate?
I wanted to be a scientist and I thought majoring in biology would be the best way. I took the medical school entrance exam to make my parents happy. I passed in Santos, but I rebelled and enrolled in biology at Unicamp in 1972. My parents wanted me to enroll at Unicamp to make their lives easier, because it would have been really hard to support me anywhere other than Campinas, where I was born and we lived. In 1973, Sidney Arcifa, a hematologist, offered me an internship at the PrevLab clinical laboratory, which had the contract to do the lab tests for Álvaro Ribeiro children’s hospital and the Campinas Medical Center. One year later, I was working the nightshift there and studying in the daytime. There was a meningitis epidemic, and I would rush from one hospital to another in the PrevLab van. I’d just barely get there, take a look at the fluid sample to be evaluated, and immediately know that the hospitalized child was in serious condition. Normal fluid is as clear as water, and what I saw would be cloudy and purulent. I’d run the tests, rush to the hospital with the report for the doctor, but by the time I got there, the child was dead. It was a very sad time; many children died.
And then?
I graduated from college in 1975 and started on my master’s in ecology, but I had to work nights at the lab. I was married by then, and my wife forced me to choose: either study or work. I dropped out of the master’s program and continued working at the lab but switched to days. The Medical Center passed the contract over to Dr. Vitor Ramos de Souza and I was promoted to assistant director. Vitor let me go back to my studies at Unicamp, and I began an internship with the immunologist Antonio Carlos Corsini. I ran experiments with him three days a week, studying the evolution of Toxoplasma gondii infection in mice and developing immunoassays [a technique for detecting antigens or antibodies]. And on the other days, I used what I learned in the laboratory at the Medical Center. Toxoplasma was important in my life.
Why?
I’d see polar staining under the microscope because Toxoplasma is shaped like a half-moon. I began reading about polar staining and came across the work of Alexander Sulzer, a researcher at the CDC [Centers for Disease Prevention and Control] in Atlanta. With Vitor’s help – since my written English wasn’t very good – I wrote to Sulzer, who replied very kindly, suggesting experiments and giving me some career advice. We exchanged letters for several years, until 1979. One day I asked him about a possible internship and he invited me to be a researcher at the CDC. By then I had remarried; my wife was a doctor and she wanted to spend some time abroad too. So we started saving up to live in the States. To avoid paying rent, I took my dad up on his offer to live above his shop – an auto parts store – in an industrial area of Campinas. Almost three years later, we had put away $14,000 – a fortune, and enough to survive at least a year in the States. And on March 3, 1980, we moved to Atlanta.
How did life go there?
I was absorbed at the CDC and my wife, at Emory University Hospital. The CDC had just wrapped up some major research projects, including identification of the bacteria responsible for Legionnaires’ disease. We started doing a lot of serologic testing of blood samples from gay men in San Francisco, looking for Toxoplasma. It was the advent of AIDS, and nobody knew what it might cause. I learned a lot about infectious diseases, and then an opportunity opened up to do my master’s at the University of North Carolina. The trouble was that our money was running out.
Didn’t you have any grant money?
I hadn’t gotten a grant in Brazil because I was an independent researcher at a private laboratory, with no ties to any university. But I got lucky. I went to the conference on tropical medicine in 1980 right there in Atlanta, with my colleague José Mauro Peralta, who was an intern at the CDC then, like me, and who is now a professor at the Federal University of Rio de Janeiro. At the conference, he ran into a physician he knew from Goiás, whose name I wish I could remember, because he really helped me out. The doctor took pity on my situation, what with my internship ending and no way to do my master’s. He said I needed grant money to get by and told me, “I’m going to introduce you to Dr. Paulo Machado.” He was talking about Paulo de Almeida Machado, who worked in tropical medicine and parasitology; he’d been Brazilian health minister [1974-1979] and was there at the conference. He was really nice, heard me out, and gave me some guidance: “Write up your work plan, send it to me, and submit a regular grant application to the CNPq [National Council for Scientific and Technological Development].” Sulzer helped me put my application together and I received a CNPq grant to do my master’s work at the University of North Carolina. I can still remember the day when I piled our things into a trailer behind our car and my wife and I merrily drove off to Chapel Hill, 500 kilometers from Atlanta, knowing I was embarking on a new phase of my life. I spent May to September back at the CDC doing experiments. Soon after that, I did my doctorate, with a dissertation on malaria, and finished up in July 1984.
Was it time to return to Brazil?
I’d received a proposal to work at the Institute of Tropical Medicine in São Paulo and another to do postdoctoral work at the Walter Reed Army Institute of Research, but didn’t accept either. I was at a conference in Texas in December 1983, when Sulzer called me to say that a staff member from the Brazilian Health Ministry had telephoned to ask about an Eduardo Franco who did cancer research. Since I didn’t know anything about cancer, I figured it must have been a mistake. But then I decided to check it out and discovered that a call had really been made, at the request of Ricardo Brentani. He was looking for an epidemiologist to work at the São Paulo branch of the Ludwig Institute for Cancer Research, which had just opened up, with him as its first director. Humberto Torloni, who had hired Brentani, had asked the ministry for the names of researchers with backgrounds in epidemiology. They gave them my name because of the CNPq grant. I talked to Torloni from Atlanta and told him I didn’t know anything about cancer. He said, “No problem. You work with infectious diseases. Did you know that one type of cancer, cervical cancer, can be caused by a virus?” I said, “I had no clue.” But they wanted to interview me. They paid for my flight and I went, in early 1984, figuring they’d see that I wasn’t the person they were looking for. I gave a seminar on infectious diseases for department heads and I noticed some of them nodding off as I spoke – they must have found it really boring. I went back to Atlanta thinking nothing would come of it, but Brentani called back with a job offer. “I liked your conscientiousness, your experience, and your ambition. I’ve got a good nose for choosing people and it’s you I want,” he said. The salary was really good and the contract included a clause – also hard to refuse – stipulating that I had to do a postdoctoral fellowship outside Brazil to learn about cancer, paid for by them. I finished my PhD and began my postdocs, the first at Louisiana State University in New Orleans; the second at the National Cancer Institute in Bethesda, Maryland; and the third at the International Agency for Research on Cancer in Lyons, France. My wife and I moved back to São Paulo in November 1984 and I started planning what to do.

Personal archives
Ricardo Brentani, Lourdes Marques, and Franco at the Ludwig Institute in São Paulo in 1990Personal archivesHow did you become an expert on HPV?
I worked with head and neck cancer and children’s cancer, but cervical cancer was a particularly serious problem. I worked with Manuel Carvalho, head of cancer reporting in Recife, and I was astonished by the rate in Northeast Brazil – more than 100 new cases for every 100,000 women every year. The cumulative lifetime risk of developing cervical cancer was 10% for any woman born in Recife. Luisa Villa, who was by then working with the virus at Ludwig, and I conducted a series of studies to determine the prevalence of women with HPV in João Pessoa, Goiânia, and Recife. It still wasn’t at all certain that the virus caused this cancer, just a suspicion. The thought was still that the herpes virus might cause this type of cancer. It was only possible to do the study in different state capitals in Brazil because Torloni introduced us to the hospital directors in the cities we visited. In 1988, after presenting our preliminary findings in Montreal, I heard about an opening at the University of Quebec. My wife liked the idea because she didn’t enjoy living in São Paulo. So I applied, got the job, and we moved, but I continued to collaborate with Luisa Villa, who has always been a marvelous colleague. We planned a study to determine the persistence of HPV infection over time, initially funded solely by Ludwig and later by the NIH [National Institutes of Health]. The Ludwig-McGill study – it wasn’t called that yet – got underway in November 1993, when we enrolled the first woman at Vila Nova Cachoeirinha Hospital in São Paulo; the last one was enrolled in 1997. The study ended in 2004, and it covered 2,528 patients ages 18 to 60, who we followed for nearly 10 years. It was one of the first longitudinal studies in the world that showed persistent HPV infection to be the prime cause of cervical cancer. We’ve continued to benefit from this research, because we kept the cell and virus samples that were collected.
What have you been doing in Canada lately?
I’ve been taking part in campaigns to persuade provinces to adopt the molecular method for cervical cancer screening. I’m also writing for the general public. One example: after spending hours working out a text on prevention with the publisher of the blog Health Debate, the results were wonderful. Then I was called, and I assembled 14 other Canadian leaders in this field. We drafted a document nearly 30,000 words long, advancing arguments in favor of changing cancer screening methods, and we sent it to every province’s health department. I’ve already met with health teams from the provinces of Ontario and Quebec. I’m in a pragmatic phase, prioritizing applied research on new methods of cancer control for the bulk of the population. One of them is self-sampling: women collect their own cell samples from their cervixes for screening, rather than having to go to a clinic.
Is this already possible?
One of our studies, CASSIS – which stands for Cervical and Self-Sample In Screening – derives from a proposal by a talented engineer from Toronto, Jessica Ching, who designed a device called the HerSwab to collect cervical cell samples for screening. It’s a pouch that contains an anatomically designed device that the woman takes home, inserts into her vagina, rotates the tip to collect the cells, puts back into the pouch, and mails off for testing. We assessed it on more than 1,000 women and found that self-sampling works much better than the Pap. Another example of applied research is gel, because although the vaccine is good, it’s still expensive and only protects against some types of HPV.
What’s the gel made of?
It’s made of carrageenan, a polysaccharide extracted from red sea algae. This work stems from a presentation I attended in 2006, by John Schiller, a scientist at the NIH who had observed that carrageenan attaches to surface receptors in HPV in vitro, which in turn attaches to the host cell, even at low concentrations. From there, the question followed: could it prevent the binding of HPV to epithelial cells? We designed the CATCH study – acronym for Carrageenan-gel against Transmission of Cervical HPV – but it took us two years to get going because we had to prove that the gel was safe to use. CATCH is a randomized clinical trial involving 500 women. Half of them will use a carrageenan gel and the other half a placebo gel. Both will apply the product before engaging in sexual relations, and they’ll come back periodically so we can see if they develop fewer cases of HPV. We expect to present our findings at an HPV conference in South Africa in late February 2017. It will be great if the gel has an impact, because carrageenan is a plentiful raw material, the patent has run out on the method for producing it, and final costs should be very low. We’re also assessing the efficacy of the gel on gay and bisexual men, both with and without HPV, at a number of research centers. The impact may be quite significant. Just think of it: a simple gel that protects against all types of HPV, even though it doesn’t act against HIV.
What about your battles against predatory journals?
In recent years, I’ve taught a number of courses – some in Brazil – on good practices in science journal publications. The open-access movement has expanded access to scientific publications since 2000, but it has created a monster: predatory journals, which have no professional ethics but do have enticing names and false addresses in the United States or Britain. They invite gullible authors to publish and, of course, charge for it. There’s no quality control. The success of these predatory journals has spread to scientific pseudo-conferences, which attract researchers who are eager to show off their work; but later, when they accept the flattering invitations, they find out they have to pay to attend. The biggest disappointment comes later, when they get to the conference and find only a handful of others, who also took the bait. We have to boycott dishonest publications to keep unsubstantiated information from passing as scientific fact. In early January, I forwarded an email to the team in my department warning about predatory journals, with this recommendation: “Protect your name and your reputation.” Another crusade is the campaign against guns. I edited a special issue of the journal Preventive Medicine, dedicated to my father, who was shot twice during an armed robbery at his shop and died in 1998. The issue came out in September 2015 and it featured great articles on the scope of gun violence, which nobody really had a handle on. One of the articles shows that gun suicides would drop 15% if gun control were greater in the United States, where 10 million people are estimated to have firearms at home. We haven’t managed to organize yet to help solve the gun problem. Crime is a public health matter too.

