In Brazil, one in every three intensive care unit (ICU) beds is occupied by a patient with sepsis, a disjointed response of the immune system activated in response to an infection. It is estimated that some 420,000 people are admitted to hospital with the syndrome every year in the country, with almost 230,000 dying. Published in The Lancet Infectious Diseases in 2017, these calculations result from the first study across a representative sample of 227 Brazilian ICUs in all regions, which evaluated the frequency of sepsis cases and related deaths. The significant mortality rate for this condition in Brazil, around 55%, is much higher than that of wealthier nations (26%), and this number has been stagnant for more than a decade.
“The current mortality rate for sepsis in the country is similar to the 2000 estimate,” says critical-care physician Luciano Pontes de Azevedo, of the Albert Einstein Hospital (HIAE), which coordinated the 2017 research in partnership with infectologist Flávia Ribeiro Machado of the Federal University of São Paulo (UNIFESP).
Mortality rates observed among adults are not dissimilar to that among children and teenagers, though the frequency of sepsis is lower among the latter. There are an estimated 75 cases for every 100,000 children (against 290 per 100,000 adults), totaling 42,000 cases per year. However, the mortality rate has remained at 20% for almost three decades. “In the 1960s the child mortality rate for sepsis exceeded 60%. We managed to reduce it to 20%, but it has not decreased any further,” says critical-care doctor Daniela de Souza, of the São Paulo University Hospital (HU-USP). Souza currently chairs the Latin American Sepsis Institute (ILAS), and is the lead author of a study published in The Lancet Child & Adolescent Health in 2021, which examined the frequency of sepsis in Brazilian pediatric ICUs.
Certain characteristics of the healthcare system help to explain these numbers. One is the lack of adequate care and monitoring from the moment at which the person with sepsis arrives at hospital. Given the high mortality rate in ICUs, Azevedo and Machado decided to investigate what happened at emergency health centers, the entry point for admissions. For three days they and their team recorded suspected sepsis cases in the emergency sector of 74 Brazilian healthcare institutions.
Of the 331 people having a condition consistent with sepsis treated at emergency centers, only 53% were referred within 24 hours to infirmaries or ICU beds, which have better conditions to treat serious cases. Due to a lack of ICU vacancies, 39% of sepsis patients treated in public institutions remained in the emergency facility throughout their admission, which in some cases lasted 13 days, and a little more than half (55%) died in those facilities. In private institutions, 9% remained in the emergency facility according to the survey results, published this year in the journal Internal and Emergency Medicine. “Treating sepsis cases in emergency facilities is inadequate. They are not set up to provide the monitoring that these patients need,” states Azevedo.
In addition to receiving care in inappropriate conditions, the specialists cite two other factors that may hamper the start of treatment: the public does not know what sepsis is, and healthcare professionals have difficulties identifying it, as the symptoms may be confused with other conditions (fever, tachycardia, shortness of breath, and mental confusion). An ILAS survey conducted years ago on 2,126 people across 134 Brazilian municipalities demonstrated that 93% had never heard of sepsis and did not know what to do about it, yet 98% knew what a heart attack was and that they should seek medical assistance — despite the mortality rate of the latter being 10 times lower than that of sepsis. “Delaying diagnosis and commencement of treatment increases the risk of death,” Souza comments.
49 million cases of sepsis occur per year around the world, according to recent estimates
Certain initiatives have demonstrated that death by sepsis can be reduced. Between 2004 and 2015, a group from ILAS assisted 63 Brazilian hospitals (25 public and 38 private) in setting up teams to deal with sepsis and implement procedures formulated by an international commission of specialists to reduce the death rate. These are standardized measures that need to be adopted during the first six hours after admission, with monitoring and control of blood pressure, assessment of tissue oxygenation levels, blood work to identify the presence of infectious agents, and administration of antimicrobials.
Over four years of monitoring, the death rate in these hospitals fell from 54% on average to 39%, according to data published in 2017 in the journal Critical Care Medicine. The impact was greater and longer lasting in private institutions, where the rate fell from 48% to 27%, and lower (from 61% to 55%) and more short-lived in public facilities, which generally have fewer resources and ICU beds, and smaller care teams. “To change the current rates, awareness on the relevance of the issue needs to be raised among the population, healthcare professionals, hospital administrators, and the public authorities,” says the ILAS chair.
This is an international public health issue. After all, it is calculated that 20% of deaths around the globe result from sepsis. Every year some 49 million cases and 11 million deaths are reported, according to estimates published in The Lancet in 2020. Forty percent of cases occur in children below the age of 5.
“Mortality due to sepsis can be significantly reduced in Brazil and other countries with the very tools we have available today,” says infectologist Reinaldo Salomão, head of the Sepsis Research Laboratory at the Federal University of São Paulo (UNIFESP), and one of the founders of ILAS. He speaks from more than 30 years’ experience studying sepsis, and has seen promises of more effective treatments being made and then ruled out after proving inefficient. Since he became interested in the topic back during his medical residence, Salomão has witnessed three changes in the concept of sepsis.
In its oldest definition, applied for decades, sepsis was considered to be a generalized infection. The pathogenic agent (bacteria, fungus, virus, or other microorganism) spread through the organism, which, in attempts to fight it, generated inflammation throughout the entire body. This idea began to gain ground in the 1980s, when it was discovered that communication molecules (cytokines) released by the immune cells could activate an inflammation spread, even if the infection remained restricted to one organ.
The focus then moved to inflammation, and in 1991 a group of international specialists proposed the following concept for sepsis: systemic inflammation arising from an infection. Ten years on, the concept was refined to better characterize severity levels and define symptoms and laboratory criteria to indicate the degree of damage to the organs. On testing strategies to control this inflammation, however, physicians realized that the phenomenon was much more complicated. Some people responded to the infection with heightened inflammation, while others presented a reduced inflammatory response. In 2016 sepsis came to be understood as an organic dysfunction with risk of death, caused by a deregulated response to infection by the host.

Bloomberg / Getty ImagesMedical team with patient at an ICU, the most appropriate environment for monitoring sepsisBloomberg / Getty Images
“These changes have been important to incorporate new knowledge into the concept, and guide the quest for therapeutic targets,” says Salomão. “Over all this time, we have discovered that patients are heterogeneous and respond to infection according to their genetic characteristics, age, and preexisting illnesses. We also learned that sepsis involves the simultaneous modulation of genes that coordinate biological processes to tackle infections, and others that attempt to prevent tissue damage,” reports the researcher, who discusses these ideas in a 2019 publication in the Brazilian Journal of Medical and Biological Research.
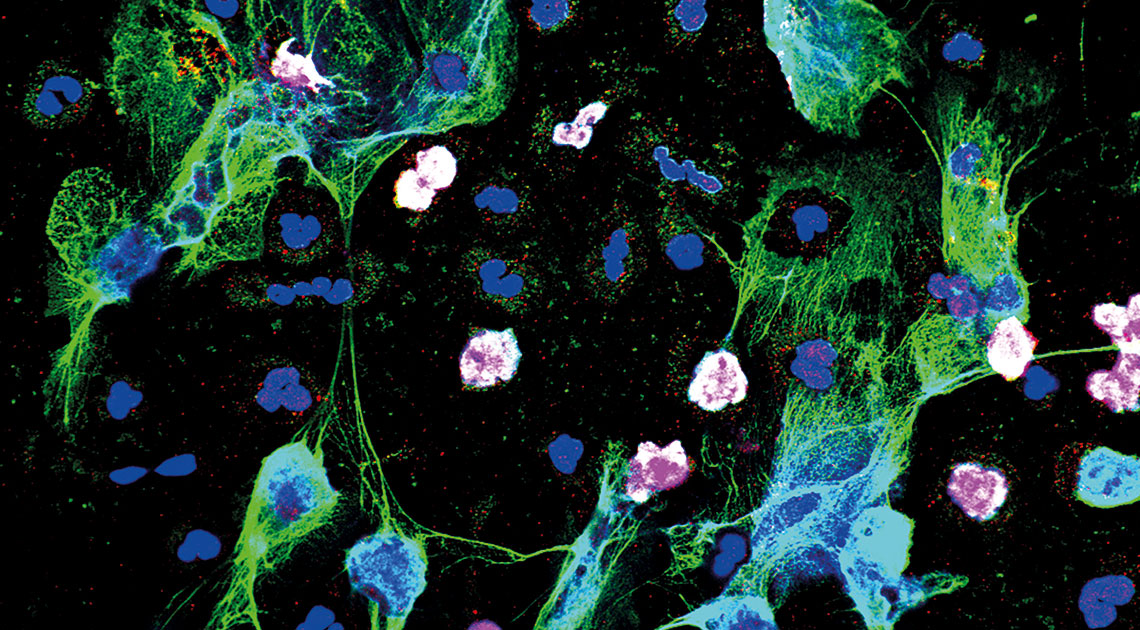
At UNIFESP, Salomão and his team conduct experiments on isolated immune cells from the blood of patients with sepsis in order to understand which phenomena represent a dysfunctional response of the organism — and, in principle, need to be tackled — and which indicate an attempt to adapt to a hostile environment and can be stimulated.
In a recent contribution the group found that, at the onset of sepsis, immune-system cells adopt an apparently less efficient strategy for producing energy, but which favors the elimination of infectious agents. Biomedical physician Bianca Lima Ferreira identified this alteration in cell function on comparing the production of monocyte and lymphocyte proteins extracted from the blood of patients at two different moments: on the day of admission, and one week later.
In the absence of infection, these cells, along with the others in the body, use glucose from foods to produce energy through cell respiration, a chemical process that consumes oxygen and generates 32 molecules of adenosine triphosphate (ATP), the fuel for cells. Ferreira noted that, right at the outset of infection, monocytes and lymphocytes in people with sepsis had deactivated cell respiration and were producing energy through anaerobic glycolysis, as observed by researchers in Rio de Janeiro shortly before. While only yielding two ATP molecules, this process is faster and prevents the consumption of ingredients that feed into the production of reactive oxygen types, compounds used to tackle invasive elements, and in the production of cytokines — messengers that attract other immune cells to the place of infection.
One week later, the monocytes and lymphocytes reduced the use of glycolysis and cytokine production, which may prevent damage to healthy cells, as reported by researchers in a 2022 article in Frontiers in Immunology. “This deactivation appears to be an attempt to return to normal, and not exhaustion of the cell, as most of these patients survived sepsis,” says Ferreira.
In another study, conducted in partnership with immunologist Tom van der Poll’s team, of the University of Amsterdam in Holland, bioinformatics specialist Giuseppe Leite analyzed the expression profile of genes and production of proteins by a wider range of immune cells found in the blood of people with sepsis. Published in 2021 in Frontiers in Immunology, the results indicated both an increase in activity among cells forming part of the first line of defense, such as monocytes and neutrophils, and suppression of lymphocytes — immune-system cells that start to act during a second stage of infection. “We demonstrated that, for sepsis, the two phenomena occur simultaneously,” explains Salomão.
11 million people die annually from the syndrome: 20% of deaths globally
While the UNIFESP group works to find the immune-cell response capacity, a team led by immunopharmacologist Fernando de Queiroz Cunha, of the University of São Paulo (USP) at Ribeirão Preto, is investigating how the action of the immune system, in addition to destroying the agent causing the infection, damages the organism itself and aggravates the situation. Over the last two decades, he and his collaborators have identified at least two mechanisms that harm healthy tissue.
The first, detailed in articles published between 2006 and 2010, is the production of nitric oxide (NO), a highly reactive molecule that interacts with cell structures and damages them. Different immune-system cells synthesize NO and deploy it against pathogens. In the case of sepsis, however, this production reaches levels a thousand times higher than normal, hampering the development of immune cells, drastically lowering blood pressure, and damaging the cells of organs such as the heart (see Pesquisa FAPESP issues 146 and 172). More recently, Cunha’s team found a second mechanism: the release of extracellular traps by neutrophils, immune cells abundant in the blood, and one of the first to migrate to the focus of infection. On encountering a pathogen, the neutrophil envelops it and emits a corrosive stream of nitric oxide upon it. If the situation gets out of control, signals from the environment lead the neutrophil to unravel its DNA and, in an explosive, suicidal event, launch it, soaked in toxic compounds, against the invaders.
In experiments simulating sepsis in mice, pharmacologist Paula Czaikoski found that the release of these DNA traps was one of the lesion mechanisms in the organs. Its production increases significantly after the onset of infection — something also observed in the blood of people with sepsis — as occurs with tissue damage. Infections and lesions were only controlled using an antibiotic associated to an enzyme that degrades DNA and is used to treat cystic fibrosis, according to results published in the journal PLOS ONE in 2016. “This and other ways of attempting to undo these traps are being evaluated in clinical tests,” says Cunha. His group, which participated in the USP task force to study COVID-19, demonstrated, in a 2020 article published in the Journal of Experimental Medicine, that this is also the mechanism behind some pulmonary lesions caused by the novel coronavirus.
Alongside the identification of these mechanisms, immunopharmacologist José Carlos Alves Filho and biomedical physician Daniele Nascimento discovered two causes of lasting immune suppression observed in sepsis survivors. One, described in 2010 in Critical Care Medicine, is the proliferation of regulatory T lymphocytes, immune-system cells that suppress the inflammatory response and deactivate other immune cells. Damaged tissues release cytokines that activate repair mechanisms and stimulate the multiplication of these lymphocytes. In the journal Immunity, the pair demonstrated in 2021 that a subpopulation of B lymphocytes releases high doses of a compound that deactivates macrophages, cells that encompass and destroy pathogens. “In experiments with rodents, these B lymphocytes remained active for a long time,” reports Alves Filho.
Despite advances in understanding the mechanisms involved in sepsis, treatment is not set to change very soon. For now, say the specialists, the most effective approach remains to fight the infection with antimicrobials as quickly as possible to prevent it getting out of control, which by itself would be sufficient to reduce mortality rates.
Projects
1. Sepsis: mechanisms, therapeutic targets, and epidemiology (nº 17/21052-0); Grant Mechanism Thematic Project; Principal Investigator Reinaldo Salomão (UNIFESP); Investment R$3,614,841.78.
2. Sepsis: integrating basic research and clinical investigation II (nº 11/20401-4); Grant Mechanism Thematic project; Principal Investigator Reinaldo Salomão (UNIFESP); Investment R$2,930,179.02.
3. Impact of implementing a managed care protocol for sepsis mortality in public hospitals in the state of São Paulo (nº 09/53227-70); Grant Mechanism Research Grant – Public Policy Research for the SUS; Principal Investigator Flávia Ribeiro Machado (UNIFESP); Investment R$95,519.45.
4. CPDI – Center for Research into Inflammatory Diseases (nº 13/08216-2); Grant Mechanism Research, Innovation, and Dissemination Centers (RIDCs); Principal Investigator Fernando de Queiroz Cunha (USP); Investment R$67,979,975.52.
5. Mechanisms involved in the pathophysiology of rheumatoid arthritis, pain, and sepsis (nº 11/19670-0); Grant Mechanism Thematic project; Principal Investigator Fernando de Queiroz Cunha (USP); Investment R$4,156,944.81.
6. The role of ectonucleotidase CD39 in the establishment of sepsis-induced immunosuppression (nº 15/25974-3); Grant Mechanism Postdoctoral Fellowship; Supervisor José Carlos Alves Filho (USP); Beneficiary Daniele Carvalho Bernardo Nascimento; Investment R$222,554.85.
Scientific articles
MACHADO, F. R. et al. The epidemiology of sepsis in Brazilian intensive care units (the Sepsis PREvalence Assessment Database, SPREAD): An observational study. The Lancet Infectious Diseases. vol. 17, no. 11, pp. 1180–89. nov. 2017.
DE SOUZA, D. C. et al. The epidemiology of sepsis in paediatric intensive care units in Brazil (the Sepsis PREvalence Assessment Database in Pediatric population, SPREAD PED): an observational study. Lancet Child & Adolescent Health. vol. 5, no. 12. dec. 2021.
MACHADO, F. R. et al. Sepsis in Brazilian emergency departments: a prospective multicenter observational study. Internal and Emergency Medicine. vol. 18, pp. 409–21. feb. 2, 2023.
MACHADO, F. R. et al. Quality improvement initiatives in sepsis in an emerging country: Does the institution’s main source of income influence the results? An analysis of 21,103 patients. Critical Care Medicine. vol. 45, no. 10, pp. 1650–9. oct. 2017.
RUDD, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. The Lancet. vol. 395, no. 10219, pp. 200–11. jan. 18, 2020.
SALOMÃO, R. Sepsis: Evolving concepts and challenges. Brazilian Journal of Medical and Biological Research. apr. 15, 2019.
FERREIRA, B. L. et al. Glucose metabolism is upregulated in the mononuclear cell proteome during sepsis and supports endotoxin-tolerant cell function. Frontiers in Immunology. nov. 18, 2022.
LEITE, G. G. F.et al. Combined transcriptome and proteome leukocyte’s profiling reveals up-regulated module of genes/proteins related to low density neutrophils and impaired transcription and translation processes in clinical sepsis. Frontiers in Immunology. sept. 10, 2021.
CZAIKOSKI, P. G. et al. Neutrophil extracellular traps induce organ damage during experimental and clinical sepsis. PLOS ONE. feb. 5, 2016.
VERAS, F. P. et al. SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathology. Journal of Experimental Medicine. sept. 14, 2020.
NASCIMENTO, D. C. et al. Role of regulatory T cells in long-term immune dysfunction associated with severe sepsis. Critical Care Medicine. vol. 38, no. 8, pp. 1718–25. aug. 2010.
NASCIMENTO, D. C. et al. Sepsis expands a CD39+ plasmablast population that promotes immunosuppression via adenosine-mediated inhibition of macrophage antimicrobial activity. Immunity. vol. 54, no. 9, pp. 2024–41. sept. 14, 2021.