NUCEL / CELLPROTECTMicrocapsules with pancreatic islets: without immunosuppressionNUCEL / CELLPROTECT
Last December 16 there was reason for an early celebration at Nucel, the Center of Cellular and Molecular Therapy at the University of São Paulo (USP), even though Christmas was still nine days away. CellProtec, a young biotechnology firm that resulted from research started at Nucel (a spin-off in economic jargon), filed its first patent request with the National Institute of Industrial Property (NIIP). The target of intellectual protection was a new formulation of microcapsules that might elevate the transplant of pancreatic islets, currently still an experimental procedure and therefore subject to many restrictions, to the status of an effective and safe diabetes treatment, in particular for type 1 patients, who produce no insulin at all and depend on regular injections of this hormone to control the disease. Made from alginate, a material obtained from brown algae, the capsules are used to coat the islets, which enables transplants without reducing the immune defenses of the recipient using drugs.
The first problem in this sort of implant, which involves taking cells from the pancreas of a newly deceased human donor, is to control rejection. Suppressing an implant recipient’s immune system is an expensive and delicate procedure that makes the sick person particularly frail and predisposed to catch infections. The second is keeping the islets, the site of the beta cells, responsible for producing insulin, working properly for a long time. According to the researchers from the university and from the firm, who developed the microcapsules jointly, these two barriers can be overcome by using implants of encapsulated islets. “We have controlled diabetes in mice that received the transplant and the islets have been producing insulin for more than 300 days,” states the biologist Mari Sogayar, a senior professor at the Institute of Chemistry at USP, coordinator of Nucel and a consultant to CellProtect. “Now, we’d like to test the approach with larger animals and, if everything works out, with human patients.”
Thanks to the efforts of Mari Sogayar’s team, whose laboratory was the first and is still the only one in Brazil capable of isolating human islets, five diabetic patients have already received pancreatic cell implants since December 2002. However, in all the procedures conducted in the country so far, the injected biological material was not coated. Now, together with CellProtect, which she helped to establish along with other researchers and former graduate students, the biologist wants to take this one step further and start using the microcapsules in transplants. “We´ll be able to control the compounds that can enter and exit the pores of this coating,” says the physician and researcher from Minas Gerais, Thiago Rennó dos Mares Guia, CEO of CellProtect and Nucel collaborator. “Beta cells are very delicate and they need a suitable supply of nutrients and oxygen to stay alive.”
Because it causes few reactions in the immune system, alginate is a base compound often used to coat elements for human implants. Its use in the CellProtect/Nucel microcapsules is no great innovation. However, the distinguishing features of the Brazilian biomaterial, according to the researchers, are its unique physical and chemical properties. “It’s like baking a cake,” compares the biologist Ana Carolina Vale Campos-Lisbôa, who did her doctorate under professor Mari Sogayar and who is one of the CellProtect partners. “The way in which each person uses the ingredients makes the recipe unique.” Alginate, which in fact is also used liberally in cooking, in the form of gelatins and emulsifiers, is the result of the combination of two chemicals, guloronic acid and mannuronic acid. Mixed in different proportions, these substances result in alginates with different characteristics. The elasticity, resistance and porosity of this biomaterial vary depending on the “recipe” used.
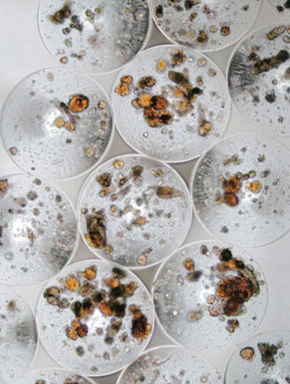
 It is unnecessary to put pancreatic islets into the microcapsules. The islets are soaked in a viscous solution of alginate and calcium and barium ions and then made to trickle through a special tap, from which they come out inside a sphere of the biomaterial. The diameter of the CellProtect/Nucel microcapsules ranges from 600 to 800 micrometers, making them large enough to house, with some slack, a group of islets within. The exact size of their pores is one of the secrets of the Brazilian team. Because of their dimensions and physicochemical properties, the tiny pores on the walls of the alginate spheres function like a selective membrane. They keep harmful elements from getting out, such as antibodies and macrophages (cells that swallow elements that are strangers to the organism), but they allow glucose, oxygen and other indispensible nutrients for maintaining the beta cells to pass through. Additionally, they also allow the insulin made by the islets to be released from within the spheres, which is essential (see figure). Thus, the hormone that the body lacked reaches the diabetic’s blood stream.
It is unnecessary to put pancreatic islets into the microcapsules. The islets are soaked in a viscous solution of alginate and calcium and barium ions and then made to trickle through a special tap, from which they come out inside a sphere of the biomaterial. The diameter of the CellProtect/Nucel microcapsules ranges from 600 to 800 micrometers, making them large enough to house, with some slack, a group of islets within. The exact size of their pores is one of the secrets of the Brazilian team. Because of their dimensions and physicochemical properties, the tiny pores on the walls of the alginate spheres function like a selective membrane. They keep harmful elements from getting out, such as antibodies and macrophages (cells that swallow elements that are strangers to the organism), but they allow glucose, oxygen and other indispensible nutrients for maintaining the beta cells to pass through. Additionally, they also allow the insulin made by the islets to be released from within the spheres, which is essential (see figure). Thus, the hormone that the body lacked reaches the diabetic’s blood stream.
International race
Biotechnology companies in various parts of the world have decided to invest in the development of biocompatible materials that might be used to coat pancreatic islet implants to treat type 1 diabetes. As encapsulating cells neutralizes the immune reaction of the body without requiring drugs, this type of transplant might, in theory, be done with healthy, insulin producing islets from a wide range of sources: human donors, animals, or islets grown in laboratories from stem cells. Living Cell Technologies, a New Zealand company, is one of the most advanced in its experiments with this approach to diabetes. It is currently holding stage 2 clinical trials, designed to find out whether the procedure works and whether it has side effects in humans, using a cellular kit called Diabecell, which contains encapsulated pancreatic islets from swine. ViaCyte, a biotechnology company from San Diego, California, is another strong competitor in this market. The company has produced and encapsulated the beta cells of pancreatic islets generated from human stem cells and it plans to test implants in patients in the near future.
This race is driven by the perception that without the aid of coating, islet transplants will remain too limited an alternative for treatment and therefore devoid of much of a future. The number of human pancreas donors is far too small to meet the needs of the huge number of patients with type 1 diabetes, who account for about 10% of all diabetics. As it is often necessary to use the pancreas of two or three donors to isolate the islets for implanting into a single receiver, the technique is hard to apply in real life. Complicating matters further, most patients have to repeat the procedure after a few years, as the islets die and stop making insulin. Then it is necessary to intervene again, by inserting a catheter in the patient’s abdomen and injecting the cells into the liver’s portal vein. “The useful life of the encapsulated islets with our material is far greater,” says Mares Guia. “And the microencapsulation reduces the cost of the implant, because one eliminates the cost of the immunsuppresants.”

VIACYTEPancreatic islets derived from stem cells within a subcutaneous device of the company ViaCyteVIACYTE
Created in 2008, CellProtect is a small company created within the university. It has three partners and four CNPq (National Council for Scientific and Technical Development) grant holders. The research is conducted at the firm’s facilities and at Nucel. Until January of last year, the headquarters of CellProtec consisted of a room at Cietec (the Center for Innovation, Entrepreneurship and Technology), an incubator of new businesses on the main USP campus in São Paulo city. Today, the spin-off, which is yet to acquire its own facilities, rents an office in São Paulo city and has a secretary to answer the phone. Is such a structure sufficient for it to compete with the foreign companies that are also investing in encapsulated islets for transplants’ Mares Guia believes it is. “Our encapsulation formulation is better than the others,” he says. “If the FDA (the government agency in charge of regulating the use of drugs and clinical procedures in the United States) approves the use of microencapsulated islets transplants to treat diabetes, we will be ready to offer a good alternative with domestic technology.”
If and when they get the green light for conducting human trials with the transplant of encapsulated islets, the Nucel and CellProtect researchers hope to be close to having a small device to implant under the patient’s skin, to be recharged with a new supply of insulin-producing cells from time to time. Thus, as soon as the implanted material became ineffective, months or years after the initial transplant, it would be unnecessary to inject a new dose of coated islets into patients’ abdomens. Instead, one would remove the dead cells from the device and replace its refill with encapsulated healthy islets, a simple procedure requiring no hospitalization. It would also mean the end of the daily insulin injections that keeps type 1 diabetics alive.
The idea may sound like a dream, but the scientists say it is feasible. They plan to create a prototype of the device this year. They also hope that as new biomaterials are developed and the encapsulation techniques progress, the need to refill the implant content’s should become rarer. “The earliest pace-makers were huge and had to be replaced in just a few months,” recalls Mari Sogayar. “Now, they last for years. We believe the same could occur with islet implants.” In the second half of the year, Nucel is expected to open new headquarters, with a floor area of 2 thousand square meters. Its construction consumed R$1 million provided by Finep (the Studies and Project Finance Agency) and another R$ 5 million provided by BNDES (the National Bank for Economic and Social Development). The building will be beneficial for the center’s research, including that done in partnership with CellProtect.
Republish