If everything goes as planned, within the next few months two women aged 30 and 35 who are unable to carry a pregnancy will undergo a uterus transplant from a deceased donor at Hospital das Clínicas (HC), of the University of São Paulo School of Medicine (FM-USP), and will then attempt pregnancy. Hopes are high after the first transplant of this kind by a team from the school’s Department of Gastroenterology was a success: the girl who was born 15 months after the transplant turned one on December 15, 2018 and, like her mother, was in perfect health.
The uterus transplant from a deceased donor at USP was the first success after around 10 attempts using the same approach in the US, Turkey, and the Czech Republic. About 39 transplants from live donors since 2013 have led to 11 livebirths. As it becomes more mainstream and accepted as a therapeutic approach in the public health system, this procedure could offer a treatment option for infertility, a condition affecting 10% to 15% of women.
“This is a major breakthrough for gynecology and obstetrics in Brazil, although its indications are very limited,” says Antonio Moron, a fetal surgeon at the Federal University of São Paulo (UNIFESP), who was not part of the study team. This type of transplant is indicated for women without a uterus due to congenital problems or surgeries.
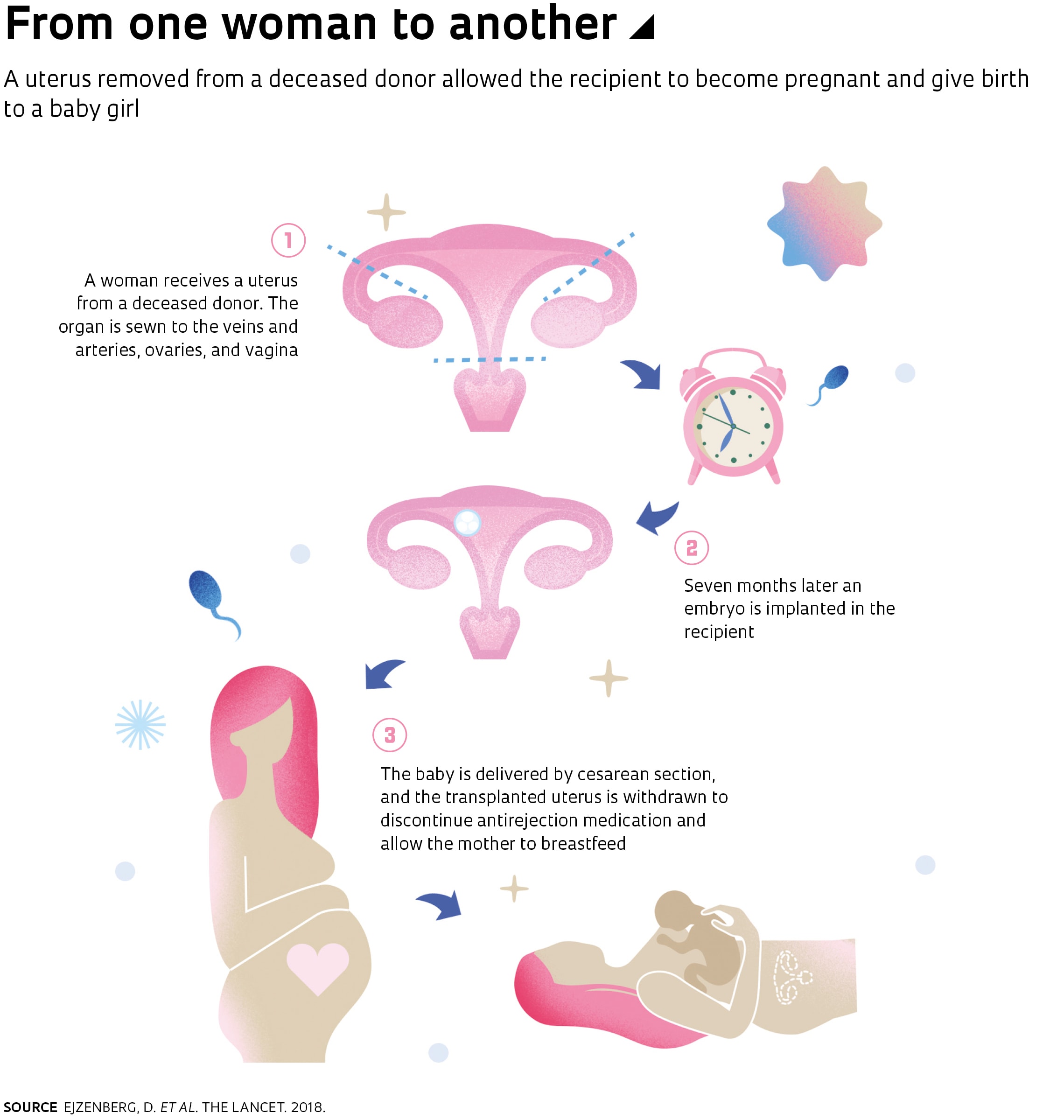
The 32-year-old woman who underwent transplantation at HC on September 20, 2016, was born without a uterus as a result of Mayer-Rokitansky-Küster-Hauser syndrome, although her ovaries produced eggs. The donor had had three naturally delivered children and had died of brain hemorrhage at age 45. The recipient first menstruated 37 days after transplantation and, two months later, became pregnant after being implanted with an embryo. One of the takeaways from the trial is the knowledge that embryo implantation can be done within less than a year of uterus implantation, the period other teams had awaited with live donors; this can lead to reduced costs on medication and medical care.
The uterus was not rejected after transplantation or during pregnancy and was withdrawn after delivery so the mother could stop taking immunosuppressive drugs and breastfeed her child, according to an article published by the HC team on December 4, 2018, in The Lancet.
“The risk of complications seems low,” says surgeon Wellington Andraus, who heads the liver transplant service at the Department of Gastroenterology at FM-USP. On his desk he keeps a photograph of the girl, who was born at 36 weeks, by cesarean section, weighing 2.5 kilograms (5.5 pounds).
“The uterus is highly resistant,” notes Andraus. The trial, which he led alongside gynecologist Dani Ejzenberg, also of USP, suggests that the pear-shaped organ can remain in good condition for eight hours after being withdrawn from the donor; this is the same survival period as for organs such as the liver and pancreas, and almost triple that of the heart.
The Brazilian Strategy
In 2015, an article in The Lancet described the first uterus transplant from a live donor in February 2013 and the delivery of a baby in September 2014, both performed by a group from the University of Gothenburg, in Sweden. After reading the paper, Ejzenberg asked Andraus if they could work together to attempt this kind of transplant. Andraus accepted. “It was clearly an innovative procedure that deserved special attention,” says surgeon Luiz Carneiro D’Albuquerque, a professor at FM-USP and head of the Liver and Digestive Organ Transplant Division at HC.
The group chose to work with deceased donors within the Brazilian organ donation program; from January to September 2018, a total of 3,625 kidneys, 1,485 livers, 266 hearts, and 31 pancreases were transplanted as part of the program, according to the Brazilian Organ Transplant Association (ABTO). This would make organ withdrawal faster and less costly than with live donors.
D’Albuquerque had to provide details on the experience of his group, which performs 120 liver transplants a year, for Ejzenberg and Andraus to be accepted into a practical course with sheep in 2016 at the University of Gothenburg. Drawing lessons from one of the cases they witnessed in Sweden—the woman could not become pregnant because she divorced her husband and he refused permission for her to implant the embryo—the HC team amended the consent form to include an ethics-based provision: the husband can make decisions together with his wife up to the time of the transplant, but thereafter it is up to the woman alone to decide whether or not to implant the embryo.
“Our work would have been impossible without the support of staff at state and national organ transplant services, who authorized the transplant and interviewed the families of potential donors,” says Andraus. As a precaution, they obtained uteruses from seven different deceased donors, generally in the wee hours of the night, after the transplant team had removed the liver and kidneys, which are given priority.
The Brazilian team presented the results of the program in September 2017 at a conference in Gothenburg. In December, a week before the girl was born in São Paulo, physicians at the University of Dallas announced the first birth in the Americas of a baby—a boy—born after transplanting a living donor’s uterus.
The short supply of live or dead donors under 45 years, and who have had children as evidence of fertility, remains a challenge. According to D’Albuquerque, after there have been more successful cases, the next battle will be making the surgery available from the Unified Health System (SUS). “It took eight years from invention for stents [expandable tubes used to unclog arteries] to be approved by the SUS,” he recalls.
Project
Uterine transplantation program at Hospital das Clínicas (FMUSP) – a pilot project (nº 16/01223-1); Grant Mechanism Regular Research Grant; Principal Investigator Wellington Andraus (USP); Investment R$149,881.68.
Scientific articles
EJZENBERG, D. et al. Livebirth after uterus transplantation from a deceased donor in a recipient with uterine infertility. The Lancet. Vol. 392, no. 10165, pp. 2697–704. Dec. 22, 2018.
BRÄNNSTRÖM, M. et al. Livebirth after uterus transplantation. The Lancet. Vol. 385, no. 9968, pp. 607–16. Feb. 14, 2015.

