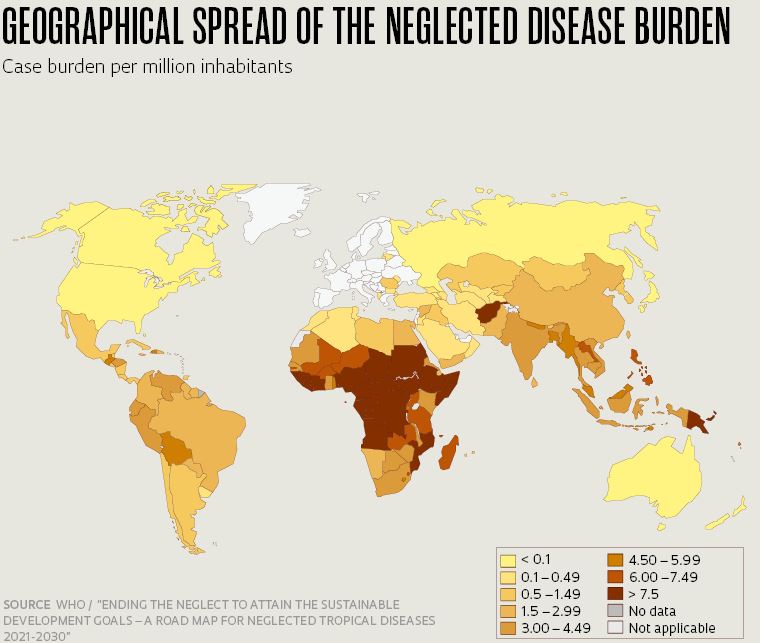
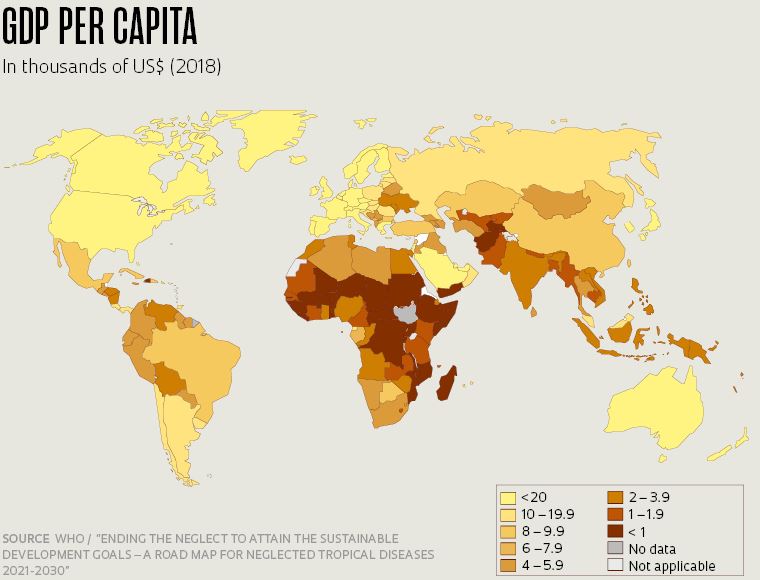
It took governments and scientists less than a year after the novel coronavirus broke out to develop and start administering a suite of seven vaccine formulations using several different technologies. But in stark contrast to the all-hands-on-deck approach to COVID-19, many infectious diseases have long plagued humanity without scientists and policymakers succeeding in efforts to eradicate or neutralize them. A report released in January by the World Health Organization (WHO) provides an update on the status of 20 such diseases, referred to as “neglected tropical diseases” (NTDs) (see chart). What these diseases have in common is that they primarily affect poor people and poor countries, which helps to explain the historically limited investment in prevention, diagnostics, and treatment.
The WHO report, developed by a group of more than 50 scientists and experts, describes progress to date since representatives from governments, pharmaceutical companies, the World Bank, the WHO, and the Bill & Melinda Gates Foundation met in London in 2012 to chart a road map for defeating NTDs. Now, eight years later, 600 million fewer people are exposed to NTDs, and 42 countries have eliminated at least one disease.
This progress was made possible by donations of 3 billion medicine tablets annually from 11 pharmaceutical companies, and by new strategies to prevent and treat NTDs in countries where they are endemic. In some cases, diseases have been successfully controlled without requiring complex measures. One example is dracunculiasis, or Guinea-worm disease (GWD), a parasitic infection that causes painful blisters on the legs or feet. In 1986, there were an estimated 3.6 million cases in African countries. By 2019 the number of cases had dropped to just 54, primarily as a result of efforts to provide clean drinking water in endemic areas.
For other NTDs, new therapies have been developed as a solution. Cases of African trypanosomiasis, also known as African sleeping sickness, fell from 7,000 in 2012 to less than 1,000 in 2019 thanks to a new oral drug, fexinidazole, developed by a consortium led by the Geneva-based Drugs for Neglected Diseases initiative (DNDi). The five drugs previously available had to be administered as an injection. Fexinidazole was first synthesized in the 1970s, but its potential use for sleeping sickness was only discovered a decade ago.

Liba Taylor / WHO
Distribution of clean drinking water in Zimbabwe in the 1990s helped to prevent the spread of dracunculiasisLiba Taylor / WHOBut despite the progress so far, the WHO estimates that at least 1.74 billion people still suffer from NTDs, and around 500,000 die annually because of them. The WHO report lays lout a new road map of measurable targets for 2030, in line with the Untied Nations’ Sustainable Development Goals (SDGs), which call to end epidemics of neglected tropical diseases over the next 10 years. The aim, as WHO Director General Tedros Adhanom Ghebreyesus put it, is to “free more than 1 billion people who currently require interventions against neglected tropical diseases.”
These ambitious targets are of course unlikely to be fully met by 2030. “The targets set are typically on the utopic side, but help to set funding priorities and can be effective in better organized countries,” says Marcos Boulos, an infectious disease specialist at the University of São Paulo School of Medicine (FM-USP), who is one of the Brazilian representatives in the working group that drafted the recommendations for the WHO report. “But often other priorities emerge and detract attention from the targets. Now, for instance, the world’s attention is fully engrossed by COVID-19.”

Christopher Black / WHO
A leishmaniasis treatment center in Kabul, AfghanistanChristopher Black / WHOThe new NTD targets call for integrated action to combat neglected diseases and for leaders around the world to work closely together to address problems. “Integration means allocating funding to healthcare using a holistic approach. Health professionals trained to administer tests for sleeping sickness also need to be prepared to identify other diseases that are prevalent in their region,” said Nathalie Strub-Wourgaft, director of neglected tropical diseases at DNDi, in an interview on the organization’s website.
One of the biggest challenges is getting funding. A survey by G-Finder, an organization that tracks research and development (R&D) investment in healthcare, showed that global funding flows for neglected diseases amounted to US$4.05 billion in 2018, a 7% increase from the previous year. But the G-Finder survey includes diseases—such as malaria, AIDS, and tuberculosis—that have commanded significant R&D funding in recent years and are no longer classified by the WHO as neglected diseases. Meanwhile, a group of six NTDs that have historically received limited funding, including leprosy, trachoma, and Buruli ulcer, saw investments decline in 2018. Malaria, on the other hand, a disease that is highly prevalent in poor countries, has been increasingly prioritized. In 2018 the Bill & Melinda Gates Foundation donated US$ 1 billion to a WHO program against malaria, and commissioned a study that developed a road map of prevention and research initiatives to eradicate the disease by 2050.

Fabio Teixeira / Agência Anadolu / Getty Images
A patient at Hospital Curupaiti, a former leper colony in Rio de Janeiro; photo taken in 2016Fabio Teixeira / Agência Anadolu / Getty ImagesThe fight against neglected diseases is largely reliant on scientific collaborations to develop new treatments. But researchers are approaching the challenge on multiple fronts. In the case of mycetoma, a disease caused by fungi or bacteria, no test is available to identify cases early enough to prevent the formation of skin deformities. Such a test could make a huge difference by enhancing the effectiveness of existing treatments. On another front, a consortium of research centers, including the Oswaldo Cruz Foundation (FIOCRUZ), is completing phase 3 clinical trials of a pediatric formulation of praziquantel, an antiparasitic drug used for treating schistosomiasis. “The existing formulation cannot be used by children under 4. The pill is extremely bitter and can cause vomiting when chewed, significantly undermining effectiveness,” explains physician Rosa Castália Ribeiro Soares, who headed the Brazilian Ministry of Health’s National Leprosy Eradication Program from 2004 to 2007 and from 2011 to 2016. She is also a member of the technical group that helped to prepare the WHO report and road map. Schistosomiasis is transmitted by contact with parasite-contaminated freshwater, and is endemic in several countries in Africa. In Brazil, schistosomiasis was a major public-health concern up until the 1970s, but was ultimately eradicated by expanding access to sanitation, health education, and treatment for affected communities, and by eliminating host snails.
The pharmaceutical industry has shown limited interest in developing drugs against neglected diseases. Because NTDs largely affect extremely poor populations, a newly developed drug would be unlikely to return a profit. A 2018 survey by researchers at Fudan University in China showed that between 2000 and 2011, only 5 of the 850 drugs approved in the US and Europe were for diseases of poverty—and all were new applications for existing drugs. “No novel medicines have yet been produced in the twenty-first century for the 20 neglected tropical diseases,” says chemist Adriano Andricopulo, from USP’s São Carlos Institute of Physics, who is developing drugs against Chagas disease and leishmaniasis.
The biggest challenge for these two diseases—both caused by the same family of pathogenic protozoa, trypanosomatids—is developing new drugs. The flagship treatments against visceral leishmaniasis are highly toxic antimonial drugs. The drug most widely used against Chagas disease is benznidazole, which is effective only if the disease is detected during the acute phase. Genomics and proteomics studies have investigated the processes that allow these parasites to survive in hosts, in order to develop drugs that can prevent infection.

Fernando G. Revilla / WHO
Spraying insecticide to kill the insect vectors of Chagas disease in the village of Palmarito, BoliviaFernando G. Revilla / WHOThree groups working on this research front met last year at the São Paulo School of Advanced Science (SPSAS) on pathogenic trypanosomatids, an event sponsored by FAPESP. SPSAS are short courses attended by researchers and young physicians from Brazil and other countries to discuss developments in the relevant research field. A new edition scheduled to be held toward the end of 2020 has been postponed to the second half of 2022. “We considered organizing an online event, but the interaction that this type of course requires depends a lot on face-to-face contact,” says Angela Kaysel Cruz, a researcher at the Ribeirão Preto Medical School at USP, and one of the event organizers.
Cruz is conducting basic research to analyze the molecular mechanisms by which Leishmania parasites undergo genetic reprogramming during their life cycles. This can help to identify targets for new drugs. She is also leading the UK: Brazil Joint Centre Partnership in Leishmaniasis, a project funded by FAPESP and British institutions such as UK Research and Innovation and the Newton Fund. The project is being co-led by parasitologist Jeremy Mottram, from the University of York. “Our partnership with the UK will explore basic questions of molecular genetics to understand the biology of the Leishmania parasite and how it regulates gene expression, and will include studies on the pathophysiology of the disease,” she says. This will be supplemented by the expertise of collaborators analyzing molecular structures and working to identify protein inhibitors.
The other two groups are also collaborating with teams in the UK. Ariel Silber, a biochemist at USP’s Institute of Biomedical Sciences, is working with researchers from the University of Glasgow to investigate how metabolism affects parasite proliferation. Adriano Andricopulo is working with colleagues at the University of Dundee. His research is looking for targets for new drugs using novel molecules from natural products derived from Brazilian biodiversity.

LQMC / IFSC
The Laboratory of Medicinal and Computational Chemistry at the Center for Research and Innovation in Biodiversity and Pharmaceuticals, in São Carlos (SP), where new drugs are being developed for Chagas disease and leishmaniasisLQMC / IFSCAndricopulo is head of technology transfer at the Center for Innovation in Biodiversity and Drug Discovery (CIBFAR), one of the Research, Innovation, and Dissemination Centers (RIDC) funded by FAPESP, and is researching 10 candidate molecules for medicines against Chagas disease and 20 for leishmaniasis. Among the most promising is a class of inhibitors of cruzain, an enzyme involved in all stages of development and differentiation of the parasite Trypanosoma cruzi. The São Carlos group is participating in an international consortium created in 2019 to develop drugs against Chagas disease, visceral leishmaniasis, and malaria. Led by Luiz Carlos Dias at the University of Campinas (UNICAMP) Institute of Chemistry, the initiative will receive funding of R$43.5 million from FAPESP and international organizations DNDi and the Medicines for Malaria Venture (MMV).
Efforts to end leprosy are also harnessing basic research to develop new medicines. Flavio Alves Lara, a microbiologist at FIOCRUZ, in Rio de Janeiro, conducted a study in 2016 to understand how Mycobacterium leprae alters the metabolism of the Schwann cells that envelop axons—which transmit electrical nerve impulses—and controls their metabolism to obtain energy. “The metabolism of the infected cell starts supplying glucose and fat to the invading bacterium rather than to the axon,” he explains. Lara is now looking to discover a molecule to block this process. “The effort may seem redundant as we can already kill these bacteria with antibiotics. But some patients still develop neuropathies during treatment and in some cases even worsen initially. So a drug that can protect the nerves during treatment, which can last for an entire year, can provide an important supplementary therapy,” he says. Lara is currently testing this approach in vitro with a compound that cannot be used clinically because of its high toxicity. “Our goal is to first produce a proof of concept and then look for more viable molecules,” he explains.
There is also a large gap for epidemiologists to fill. Efforts to combat schistosomiasis are still highly reliant on surveillance strategies such as monitoring snail populations in rivers. In a 2018 study in the journal Epidemiologia e Estudos de Saúde, Omar dos Santos Carvalho, a medical researcher at the René Rachou Institute at FIOCRUZ Minas Gerais, conducted a detailed survey to map the geographical distribution of the snail vectors of Schistosoma mansoni worms in Pernambuco, Paraná, Minas Gerais, Bahia, and Rio Grande do Norte. The data collected in the survey was fed into the databases used by health surveillance teams. The mollusks were found in 300 of the 427 municipalities surveyed. Two different species were present in 53 municipalities.

Andy Craggs / WHO
Tsetse flies, which transmit African trypanosomiasis, collected in a rural area in TanzaniaAndy Craggs / WHOBrazil has made significant strides in tackling neglected diseases such as Chagas disease and schistosomiasis. For Rosa Castália, the positive results can be partly credited to efforts on the ground within the National Healthcare System (SUS). “Training provided to primary health care professionals in the last 15 years has expanded capacity to diagnose and treat these diseases,” she says. But in the case of leprosy, perhaps counterintuitively, case numbers have not declined in recent years despite expanded efforts. “As surveillance is enhanced and access to diagnostics is amplified, more cases will be detected because infected individuals are being actively sought out and case reporting has improved,” she says. “But the sustained endemic levels are also explained by poor sanitation and other factors in transmission that are still poorly understood.” With 27,000 new cases reported in 2018, Brazil is surpassed only by India in case counts.
Flavio Alves Lara of FIOCRUZ believes underreporting alone does not explain the persistence of leprosy. “There are likely several reservoirs of the bacterium in nature—armadillos are a known example—and we have not made an effective effort to identify them,” he says. He notes that most cases are in agricultural-forest frontier regions, such as the Amazon deforestation belt. “Leprosy is neither a tropical nor an urban disease. It was prevalent throughout Europe, but local transmission fell as the region became industrialized and urbanized over time. I believe natural reservoirs disappeared in Europe, or at least their interaction with humans was reduced, during the industrial revolution. Red squirrels, which used to be hunted for their tails to make ornaments and women’s hats, are still abundant in England and have only now been identified as natural reservoirs of the disease.”

Simon Lim / WHO
Dissected snails being examined for schistosomiasis parasites in Shanghai, ChinaSimon Lim / WHOAs a member of the group developing the WHO report, infectious disease specialist Marcos Boulos found it difficult to sensitize the other panel members to problems in Brazil. “The organization’s efforts and funding are largely targeted to Africa, where neglected diseases are most prevalent.” But Brazil is by no means in a privileged position when it comes to the 20 neglected diseases. Only two of them have been shown not to occur in the country: dracunculiasis and African trypanosomiasis. Granted, Brazil is close to eradicating some NTDs. But onchocerciasis, for example, a parasitic disease that can cause blindness, is still present in Brazil’s northern state of Roraima, on a Ianomâmi reserve on the border with Venezuela. “Health workers and doctors have to trek through the jungle to find patients, as many Ianomâmi are nomadic. It appears there has been no further transmission, but this needs to be confirmed using WHO protocols,” says Rosa Castália. Lymphatic filariasis, a disease that causes swelling in the legs, has been eradicated in the states of Bahia, Alagoas, and Pará, but eradication has yet to be certified in Pernambuco, where there were active outbreaks a few years ago.
Science has an arsenal of strategies to eradicate or control infectious diseases. Vaccines, when available, are the solution of choice. It is thanks to vaccines that smallpox has been eradicated and other diseases are kept in check through periodic vaccination. The advent of antibiotics also provided the ability to treat several ancient diseases, like cholera and the bubonic plague, while the provision of basic sanitation has helped to fully eradicate them. According to the WHO, there are good prospects that a number of neglected diseases, including dracunculiasis and yaws, will be eradicated over the coming years. For other diseases, the approach taken has been to keep them at manageable levels.

Instituto Butantan
Production of a lyophilized dengue vaccine being developed at Instituto ButantanInstituto ButantanThe neglected diseases of greatest concern in Brazil today are dengue and visceral leishmaniasis. “We will continue to have annual epidemics of dengue and chikungunya because we have been unsuccessful in eliminating Aedes aegypti mosquitoes from our homes,” says Marcos Boulos. “Diseases that require the elimination of mosquito populations are particularly difficult to eradicate.” But the development of a vaccine could provide a solution. Instituto Butantan, in São Paulo, has been working on a dengue vaccine for the past 12 years (see Pesquisa FAPESP issue no. 291). Last year, close to 1 million dengue cases were reported in Brazil, with just over 500 deaths.
Another challenging disease is visceral leishmaniasis, a rural disease that was confined to Brazil’s Northeast until the 1980s, but in recent years has found its way to urban centers, including cities in São Paulo. The disease is caused by the protozoan Leishmania infantum chagasi and is transmitted by female Lutzomyia longipalpis sandflies. Infected dogs are among the reservoirs of the parasite. “These insects are not city dwellers. They live in wooded areas close to cities and it is very difficult to eliminate them. More research is needed into how the disease is spreading. In 2019, two children died of leishmaniasis in Guarujá [SP] and we have yet to track down the source,” explains Boulos. For those looking to do research on neglected diseases, there is no shortage of research targets.
The status and incidence of the 20 tropical diseases recognized as neglected by the World Health Organization
Targeted for eradication
Dracunculiasis
Dracunculiasis is a parasitic infection by the Guinea worm that causes skin ulcers, mainly on the legs. A person becomes infected by drinking contaminated water. There are cases reported in Angola, Chad, and South Sudan
Yaws
Yaws is an infection of the skin and joints caused by the bacterium Treponema pallidum pertenue. It can result in physical deformities if left untreated. Yaws remains endemic in 15 countries, such as Ivory Coast, Ghana, Papua New Guinea, Togo, and the Philippines
Targeted for interruption of transmission
Leprosy
Leprosy is a chronic infectious disease caused by the bacillus Mycobacterium leprae. The disease mainly affects the peripheral nerves, skin, and respiratory tract. Leprosy causes deformities if left untreated; 80% of new cases are in India, Brazil, and Indonesia
Onchocerciasis
Onchocerciasis is a disease caused by infection with Onchocerca volvulus, a parasitic worm transmitted by flies. It is the world’s second leading infectious cause of blindness. A total of 20 million people are affected worldwide, mainly in Africa but also in tropical regions of the Americas
African trypanosomiasis
Human African trypanosomiasis, also known as sleeping sickness, is caused by two types of trypanosomes and is transmitted by infected tsetse flies. The disease compromises the nervous system and can be fatal without treatment. Sleeping sickness occurs in southeastern and central Africa, where around 1,000 thousand cases were reported in 2019
Targeted for elimination as a public health problem
Leishmaniasis
Leishmaniasis is a disease caused by protozoan parasites that produces lesions in internal organs (visceral) and on the skin (cutaneous). The disease is transmitted by insects, with dogs as the primary reservoir of the protozoan parasites. Most cases are in India, Brazil, and Africa
Chagas disease
Chagas disease is transmitted by contact with the feces of triatomine bugs contaminated with Trypanosoma cruzi. Without treatment, it can lead to heart failure. The disease is most prevalent Latin American countries. Chagas disease killed 10,000 people in 2017
Lymphatic filariasis
Lymphatic filariasis is a disease caused by mosquito larvae migrating to the lymphatic vessels. It causes swelling in the legs and can also affect mental health. Over 50 million people are currently infected, largely in central Africa and southern Asia
Schistosomiasis
Schistosomiasis is an infection with blood flukes of the genus Schistosoma. It is transmitted by contact with contaminated freshwater, and causes symptoms such as fever and diarrhea. Although most cases are in Africa, the disease is still present in Brazil
Rabies
Rabies is a zoonotic disease that causes viral encephalitis. It is transmitted by contact with the saliva of rabid bats and dogs. Rabies is present in 89 countries, mostly in Africa and Asia. The disease caused 59,000 human deaths around the world in 2015
Trachoma
Trachoma is a disease of the eye caused by infection with the bacterium Chlamydia trachomatis. It is the leading infectious cause of blindness worldwide. The disease is present in Africa, South America, and India. In 2019, 2.5 million people required surgery for trachomatous trichiasis
Helminthiases
Helminthiases are diseases caused by intestinal parasites present in the soil, such as ascariasis, hookworm, and strongyloidiasis. Incidence rates are highest in India, central Africa, and Latin America. Helminthiases caused 6,300 deaths in 2016
Projects
1. São Paulo School of Advanced Science in Pathogenic Trypanosomatids: from biology to pathogenesis and new therapies (nº 19/17546-2); Grant Mechanism Organization for Scientific Gathering – Escola São Paulo de Ciência Avançada Principal Investigator Angela Kaysel Cruz (FMRP-USP); Investment R$547,889.14
2. Drug discovery based on the structure of the receptor and ligand for Leishmaniasis and Chagas Disease from bioactive natural products (nº 18/14268-9); Grant Mechanism Thematic Project; Agreement MRC-UKRI, Newton Fund; Principal Investigator Adriano Defini Andricopulo (IFSC-USP); Investment R$1,170,839.28
3. UK-Brazil Centre for the Study of Leishmaniasis (JCPiL) (nº 18/14398-0); Grant Mechanism Thematic Project; Agreement MRC-UKRI, Newton Fund; Principal Investigator Angela Kaysel Cruz (FMRP-USP); Investment R$2,114,545.47
4. A network for an integrative biology in neglected diseases: Connecting epigenetics, metabolism and cell biology in pathogenic trypanosomatids (nº 18/14432-3); Grant Mechanism Thematic Project; Agreement MRC-UKRI, Newton Fund; Principal Investigator Ariel Mariano Silber (ICB-USP); Investment R$3,046,521.44
5. FAPESP/MMV/DNDI/UNICAMP/USP consortium for the discovery of new medication for the treatment of tropical parasitic diseases (nº 15/50655-9); Grant Mechanism Research Partnership for Technological Innovation Program (PITE); Principal Investigator Luiz Carlos Dias (IQ-UNICAMP); Investment R$2,950,388.31
6. Center for Innovation in Biodiversity and Drug Discovery (CIBFar) (nº 13/07600-3); Grant Mechanism Research, Innovation, and Dissemination Centers (RIDC); Principal Investigator Glaucius Oliva (IFSC-USP); Investment R$32,164,849.87


