 MARIANA ZANETTIIn early January 2015, the Ministry of Health and the National Supplemental Health Agency, which regulates private health plans in Brazil, published a rule intended to reduce the number of unnecessary surgical deliveries (Cesarean sections). The measures, which are expected to begin in earnest in the second half of the year, would require doctors to justify with more rigor and detail the reasons for choosing the surgical birth of an infant. If they do not do so, they will not be paid for their work. It is an effort, considered only palliative by some physicians, to try to reduce the absurdly high rate of surgical births performed in Brazil—especially in the private health sector—and one of its likely consequences: the birth of children who have not yet reached biological maturity.
MARIANA ZANETTIIn early January 2015, the Ministry of Health and the National Supplemental Health Agency, which regulates private health plans in Brazil, published a rule intended to reduce the number of unnecessary surgical deliveries (Cesarean sections). The measures, which are expected to begin in earnest in the second half of the year, would require doctors to justify with more rigor and detail the reasons for choosing the surgical birth of an infant. If they do not do so, they will not be paid for their work. It is an effort, considered only palliative by some physicians, to try to reduce the absurdly high rate of surgical births performed in Brazil—especially in the private health sector—and one of its likely consequences: the birth of children who have not yet reached biological maturity.
Surgical deliveries are essential in cases where there is a risk of serious illness or death of the mother or infant. But, without a specific clinical indication, they may contribute, to an extent not yet known by experts, to infant births before the end of the gestation period, a phenomenon that has become increasingly common in Brazil. Doctors attending newborns are concerned about the increase in premature babies born at less than 37 weeks of pregnancy, and with so-called early terms, born at 37 and 38 weeks (see sidebar). Until recently obstetricians and pediatricians believed that early term infants had already matured enough to live well outside the womb, which is why they were considered full term. But there is increasing evidence that early terms are not yet ready to be born and that they need to spend one or two more weeks in the womb. These babies in general are discharged without any apparent complications, but they have a higher risk of developing respiratory problems—and even death—in the first days of life.
Specialists in maternal and child health suspect that there is a connection between the birth of infants who have not yet reached biological maturity and an excess of unnecessary Cesarean sections. For 40 years the rate of Cesareans has been growing in Brazil (see graph). About 15% of births were surgical in the 1970s. By the early 2000s, the number of Brazilian babies born by Cesarean had surpassed those who were born by natural means. Today 52% of the 3 million births per year are Cesarean, according to the most comprehensive study on the subject, Nascer no Brazil [Born in Brazil], whose results were published in Cadernos de Saúde Pública of the Oswaldo Cruz Foundation (Fiocruz)] in 2014. Coordinated by researchers at Fiocruz, this survey gathered information from 23,894 pregnant women in 2011 and 2012 attended at 266 hospitals (public, private and mixed) in 191 Brazilian municipalities.
Although the total number of Caesareans is higher in public hospitals—where 8 out of 10 Brazilian babies are born—they are proportionally more frequent in the private network. In private hospitals, where higher income pregnant women are attended, 90% of births are surgical, while in the public sector this figure is smaller and represents 40% of deliveries—still a high number compared to the 15% recommended by the World Health Organization (WHO). Most of these surgeries—some estimates reach 1 million—are not medically indicated, contributing to the birth of infants before they have properly matured.
Population studies conducted by various research groups at maternity hospitals in different regions of Brazil indicate that the proportion of babies born before completing 37 weeks of pregnancy has been on the rise in recent decades, a trend already observed in the United States and some European countries. The data also show that this rate—which ranges from 11% to 13% of live births, depending on the universe analyzed in the survey—is about two times higher than the official 6.5%, registered in the Live Births Information System (SINASC), of the Ministry of Health. This ranks Brazil in 10th place among countries with premature births.
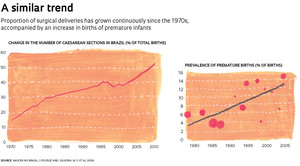 Illustration: Mariana ZanettiThe latest of these surveys, coordinated by Dr. José Guilherme Cecatti, an obstetrician at the University of Campinas (Unicamp), followed 33,740 pregnant women in 2011 and 2012 attended at 20 hospitals in the Northeast, Southeast and South. Of this total, 4,150 babies (12.3%) were born at less than 37 weeks of gestation, according to an article in the October 2014 issue of PLOS One.
Illustration: Mariana ZanettiThe latest of these surveys, coordinated by Dr. José Guilherme Cecatti, an obstetrician at the University of Campinas (Unicamp), followed 33,740 pregnant women in 2011 and 2012 attended at 20 hospitals in the Northeast, Southeast and South. Of this total, 4,150 babies (12.3%) were born at less than 37 weeks of gestation, according to an article in the October 2014 issue of PLOS One.
Not all of these premature infants were delivered by Cesarean section. In fact, most of them (65%) were spontaneous births—because the mother had not received adequate prenatal care, because she had health problems such as hypertension and diabetes, or because she was at an advanced age. In 35% of these cases, the infant was delivered prematurely through surgical intervention. Most of the time the surgery was necessary for health reasons, such as high blood pressure or problems in the placenta, which endangered the mother’s or the infant’s life. But a proportion, however small, may be due to unnecessary Cesarean deliveries. Dr. Renato Passini Junior, an obstetrician with the Unicamp group, thinks this is a difficult connection to establish. “It would be necessary to identify which C-sections were elective and then determine whether or not they were medically indicated,” he says. That is not always a simple assessment to make. “There are cases in which the indication is not absolute, and a number of conditions of the mother and the fetus may lead to the procedure, since a delay could jeopardize the health of the mother or the infant,” he says.
The strongest evidence that an excessive number of Cesareans can lead to infant births before the desired term comes from studies conducted by the pediatric team of Dr. Marco Antonio Barbieri, of the University of São Paulo (USP) in Ribeirão Preto. “We have clearly seen an increase in the rate of premature births due to C-sections, he says. In the late 1970s he started the first study of population monitoring, or cohort study, conducted in Brazil.
Barbieri and his colleagues collected data on childbirths and the health of 6,700 babies born in Ribeirão Preto in 1978 and then compared this data with the health of 2,900 babies born in 1994. During this period, the rate of premature births nearly doubled: rising from 7.6% to 13.6% of total births. The proportion increased from 30% to 51% among those born by Cesarean section in the public and private system and from 4% to 36% among those delivered in private hospitals. “The preterm birth rate doubled between the 1978 cohort and the 1994 cohort, and the proportion of premature infants born at 35 or 36 weeks tripled,” says Barbieri.
The concomitant increase in these two rates caught the attention of the researchers. “There were several factors related to the increase in the premature rate, but what stood out was the number of Cesareans,” says Dr. Heloísa Bettiol, a pediatrician and member of the Ribeirão Preto team. “By examining issues such as days of the week and the time of day when C-sections were performed, and whether or not they took place in the public or private system, we found that the convenience factor was a strong influence,” says Dr. Bettiol. According to her, this indicates that many C-sections were planned in advance, often for the convenience of the mother, the physician, or both.
A third cohort, on which data were collected in 2010 on 7,000 children, should help to more accurately estimate the rate of unnecessary Cesarean sections. “We are completing our analysis of the data collected from their medical records and interviews with the mothers who underwent C-sections,” says Barbieri. “Preliminary data show that the percentage of Cesareans scheduled and not clinically indicated is high, reaching 20% to 25% of surgical deliveries.”
 MARIANA ZANETTICaesarean sections without a specific indication do not occur only in Brazil. A survey published in the journal JAMA Pediatrics evaluated the conditions associated with 5,828 premature births in eight countries—including Brazil—and found that 4% of the infants were delivered by Cesarean for no obstetrical reason.
MARIANA ZANETTICaesarean sections without a specific indication do not occur only in Brazil. A survey published in the journal JAMA Pediatrics evaluated the conditions associated with 5,828 premature births in eight countries—including Brazil—and found that 4% of the infants were delivered by Cesarean for no obstetrical reason.
The Fiocruz study, Nascer no Brazil, also attributes what he calls “the epidemic of births at 37 or 38 weeks in Brazil” at least in part to elective surgeries, performed before the start of labor—and, therefore, with no evidence that they are necessary. According to the authors, “it is estimated that each year 1 million women in Brazil undergo medically unnecessary Cesarean sections.”
One reason why the scheduling of surgical deliveries leads to premature and early terms has to do with calculating the gestational age. “The estimated gestational age has a margin of error of plus or minus 15 days,” says Dr. Bettiol. As a result of this margin of error, if a Cesarean section is scheduled for the 37th week of pregnancy, it is possible to deliver a 35-week-old infant.
Dr. Ruth Guinsburg, a neonatologist at the Federal University of São Paulo (Unifesp), says it is important to remember that one should not demonize the Cesarean section. “When absolutely indicated, it can save the mother’s life and that of her baby,” she says. “What the government is trying to do with the new measure is to reduce the absurd number of children born at 36, 37 and 38 weeks.”
In recent years doctors have begun to worry about these babies because they tend to be discharged and go home without any apparently serious complications. But studies are showing that even those who are born at 37 or 38 weeks have a greater risk of developing health problems during the first days after birth, the first year of life and even in adulthood.
“Late preterm infants, even chubby ones who appear to be in good health, may have a number of small problems,” says Dr. Guinsburg, the head of the neonatal ICU at Hospital São Paulo, a Unifesp affiliated hospital. They have more difficulty breathing, maintaining adequate levels of glucose and electrolytes in the blood and nursing. They are also at higher risk of dying in the first year of life than children who were born one or two weeks later. One of the studies that confirm the increased vulnerability of these babies was conducted by the pediatric team of Dr. Fernando Barros, at the Federal University of Pelotas (UFPel) in Rio Grande do Sul. For almost three decades Barros and his colleagues monitored the health of almost all the children born in the years 1982, 1993 and 2004 in the city of Rio Grande do Sul.
 Illustration: Mariana ZanettiBy comparing data on pregnancy, childbirth and health, they found that babies born at 37 weeks of gestation had twice the risk of dying in the first year of life than those born at 39 weeks. The mortality rate was 23 per 1,000 in the first group and 10 per 1,000 in the second group, according to a 2012 article in the journal BMC Pediatrics.
Illustration: Mariana ZanettiBy comparing data on pregnancy, childbirth and health, they found that babies born at 37 weeks of gestation had twice the risk of dying in the first year of life than those born at 39 weeks. The mortality rate was 23 per 1,000 in the first group and 10 per 1,000 in the second group, according to a 2012 article in the journal BMC Pediatrics.
“The cutoff point used by WHO to define a full term pregnancy is inappropriate and should change shortly,” says Barros. “Several studies highlight the need to change it to 39 weeks.” Cecatti, of Unicamp, disagrees. “I think for WHO to have an official position raising the threshold of preterm births is problematic because many variables are involved,” he says.
In any case, experts recommend that mothers and their doctors schedule surgery at the 39th week of pregnancy. Or, ideally, wait until the start of labor. “Nature provides the best indication of when babies are ready to be born, with the onset of labor,” says Cecatti.
Transforming this scenario is not a simple matter. The Nascer no Brasil study shows that the health care of pregnant women is inadequate: 60% of pregnant women undergo their first prenatal examination after the 12th week of pregnancy, which is considered late, and 25% do not have the six recommended doctor’s visits. Another 60% did not receive information about which maternity hospital to use, and almost 20% had to seek care in more than one such hospital after the start of labor—generally they lacked doctors, equipment or materials.
It’s not just the public sector. The supply of obstetric beds in private hospitals continues to decline; these hospitals also lack doctors and specialized teams, including doulas and nurse midwives, for normal deliveries. “Maternity hospitals are no longer a good business and many are closing. Those remaining are surgical centers geared toward C-sections,” says César Eduardo Fernandes, a member of the Professional Defense Committee of the Association of Obstetrics and Gynecology of São Paulo (SOGESP).
There is a consensus among those interviewed for this article that the way to reduce the number of unnecessary Cesarean sections, and the birth of children not quite ready to come into the world, is to reorient the health care system when it comes to pregnancy and childbirth. “The measures announced by the National Health Agency are palliative,” says Fernandes. “Criminalizing the obstetrician will not reduce the number of C-sections. We have to invest in reeducating doctors, health professionals and patients.” Fiocruz’s Maria Elisabeth Moreira believes any change in this scenario must necessarily include the empowerment of mothers. “We need to do what has been done with breastfeeding: offer information so mothers can make an informed decision on what the best mode of delivery for them is,” she says. Even if the final decision rests with their doctors.
Projects
1. Etiological factors of preterm birth and consequences of perinatal factors in child health: birth cohorts in two Brazilian cities (No. 2008/53593-0); Grant mechanism: Thematic Project; Principal investigator: Marco Antonio Barbieri (USP-Ribeirão Preto); Investment: R$2,913,904.66 (FAPESP).
2. Multicentric study on preterm births in Brazil (No. 2009/53245-5.); Grant mechanism: Research Grant – Research in Public Policies for the National Health Care System (PP-SUS); Principal investigator: José Guilherme Cecatti (Unicamp); Investment: R$296,623.37 (FAPESP).
Scientific articles
PASSINI JUNIOR, R. et al. Brazilian multicenter study on preterm birth (EMIP): prevalence and factors associated with spontaneous preterm birth. PLOS One. October 24, 2014.
BARROS, F.C. et al. Gestational age at birth and morbidity, mortality, and growth in the first 4 years of life: findings from three birth cohorts in Southern Brazil. BMC Pediatrics. October 2012.
SILVEIRA, M.F. et al. Increase in preterm births in Brazil: review of population-based studies. Revista de Saúde Pública. October 2008.


