When new and severe cases of yellow fever were admitted at a university hospital (HC) run by the University of São Paulo School of Medicine (FM-USP) in the early months of 2018, the hospital’s medical staff soon realized they were at a loss for how to treat the disease, which is as rare in São Paulo as it is lethal—the disease can lead to death in as few as two days. As new patients continued to arrive, the medical staff quickly began to test, adapt, and implement strategies for treatment. As a result of their efforts, the mortality rate for severe cases of yellow fever was 67% for the year, compared with an expected rate of 80%.Since January this year, an enhanced version of the protocol, which includes more frequent plasma (the liquid portion of the blood) exchange, has been implemented and has helped to further reduce the mortality rate. Of the 39 patients with yellow fever admitted up to May this year, only two died. Although the results are promising, infectious disease specialist Esper Kallas of FM-USP says the reduced mortality should be viewed with caution. “The improved treatment helped, but we still don’t know whether this year’s cases were milder than last year’s,” he says.
The recent sylvatic yellow fever outbreak has been the most severe in Brazil in decades. The sylvatic form of the disease is transmitted by insects of the genera Haemagogus and Sabethes, whereas the urban version is transmitted by Aedes aegypti, although the virus is the same in both cases.
The Brazilian Ministry of Health reported 1,376 cases and 483 deaths from yellow fever from July 2017 to June 2018, with the virus reaching as far as the metropolitan areas of Belo Horizonte, Rio de Janeiro, and São Paulo for the first time. In recent months, the virus has made its way further south: an epidemiological bulletin released on June 13 by the Paraná State Department of Health reported 17 patients with the disease from July 2018 to June 2019 and one death in the coastal town of Morretes. The most recent case was reported in Quatro Barras, in the Metropolitan Area of Curitiba.
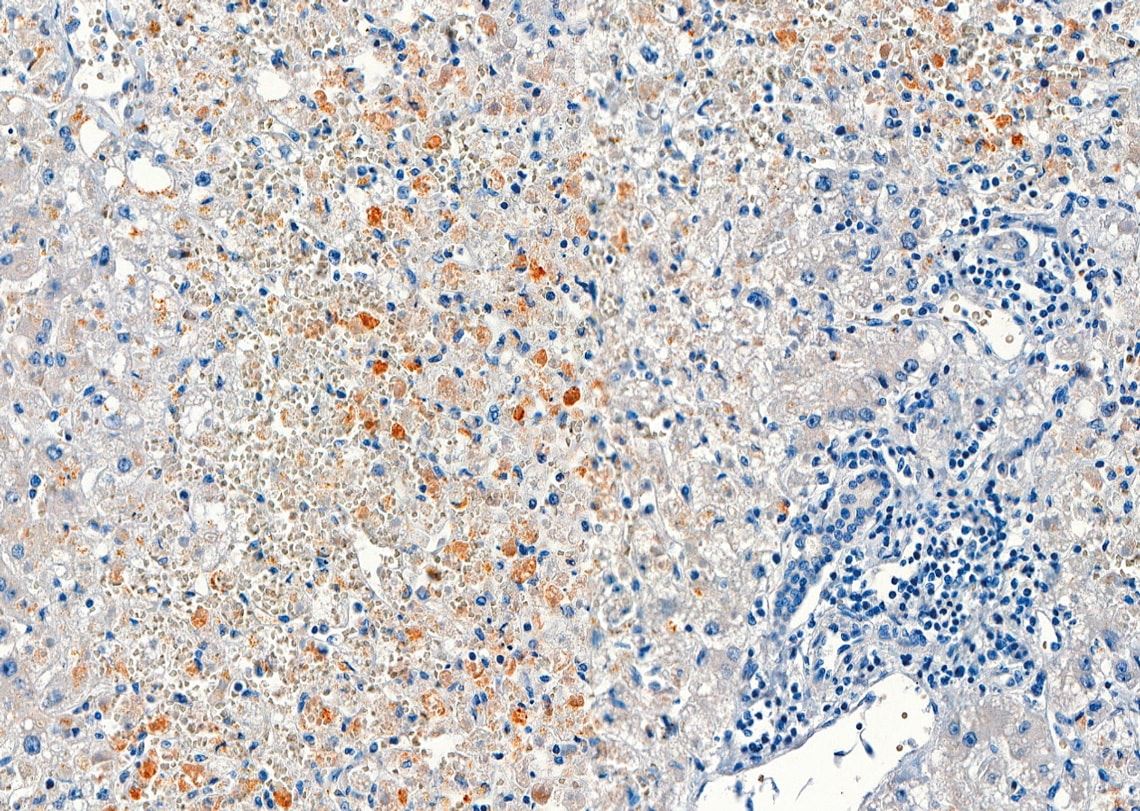
Amaro Nunes Duarte Neto / FM-USP
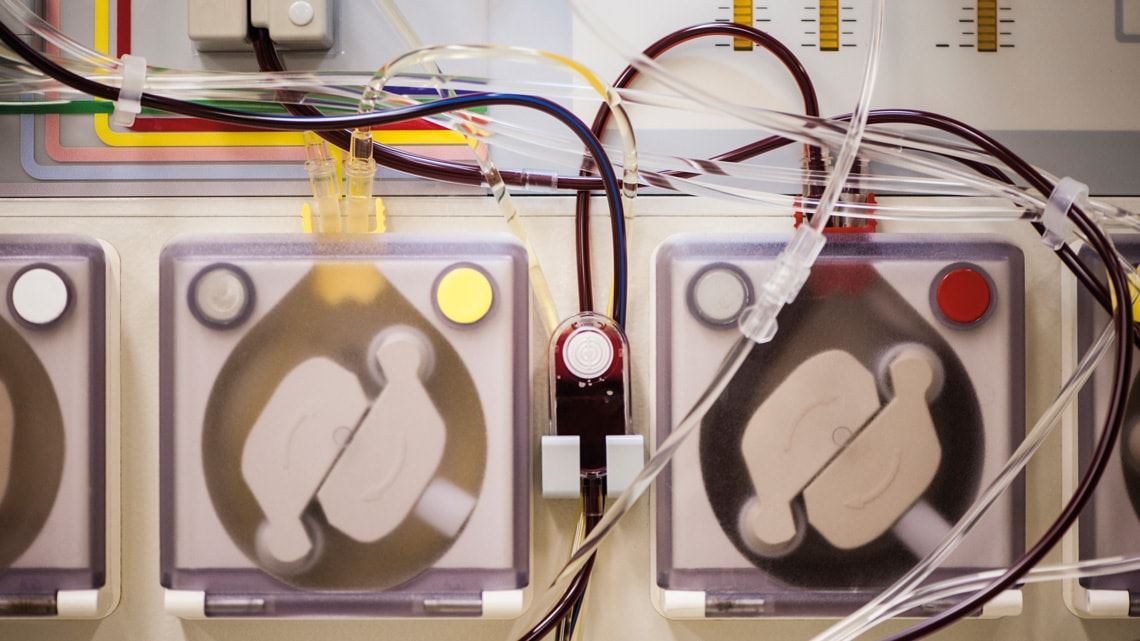
The virus causes severe hepatitis (shown in brown, liver cells with the viral antigen)Amaro Nunes Duarte Neto / FM-USPYellow fever initially causes fever, muscle aches, headache, loss of appetite, prostration, nausea, and vomiting, with these symptoms appearing as the disease-causing virus establishes itself in the body. The initial symptoms usually subside within four days, and infected people are usually unaware that they have become infected, as the first signs can be mistaken for symptoms of other diseases such as dengue fever or a passing flu. From 10% to 15% of cases develop the severe form of the disease, which can be fatal: the skin and eyes turn yellow and the turns urine dark, the fever reappears, the severity of the abdominal pain and vomiting increases, and the patient begins to present with diarrhea and bleeding. The yellow fever vaccine, produced from attenuated virus, is the most effective form of prevention against the disease.The treatment strategy adopted at HC consists primarily of plasma exchange to reduce viral load, replace coagulation factors, and thereby avert the intense bleeding that marks the final phase of the disease. In 2019, staff at the hospital’s intensive care unit (ICU) for infectious diseases and hematology decided to increase the frequency of the plasma exchange sessions, drawing from the experience gained by physicians treating yellow fever in Rio de Janeiro. Rather than administering approximately 30 plasma units once per day as they had done the previous year, they began to administer half that volume twice per day.
“Doing sessions at shorter intervals prevented patients from bleeding between sessions as before,” explains infectious disease specialist Yeh-Li Ho, who heads the UCI for infectious diseases at the hospital and is the lead author of a paper reporting the results of the new strategy, published in May in the Journal of Travel Medicine. Furthermore, she says, the shorter sessions meant the unit was able to treat more patients.
Another modification was that instead of stopping the plasma exchange sessions after three days, they were gradually diminished “until liver function was restored,” says the physician. As a result, says Ho, “we were able to contain the progression of the disease and reduce the lethality.”
One of the signs that their strategy had been successful was the normalization of lipase levels, which helped to keep the pancreatitis—an inflammation of the pancreas that is one of the complications of yellow fever—from worsening. “This year, we have had no fatal cases of severe pancreatitis in yellow fever patients.”

Amaro Nunes Duarte Neto / FM-USP
Bacteria (shown in blue) spread in the lungs and cause pneumonia (images taken with a microscope)Amaro Nunes Duarte Neto / FM-USPThe new approach has also proven to be effective at the Emílio Ribas Institute of Infectious Diseases (IIER) near HC. Earlier this year, intensive care physician Jaques Sztajnbok and his team employed plasma exchange to treat a 43-year-old man from Vale do Ribeira. Previous procedures, including hemodialysis and packed red cell transfusion, failed to contain the patient’s continuous bleeding and multiple organ failure. However, plasma exchange once per day was shown to be effective: after the third day, the bleeding stopped, and the patient recovered, as reported in a July article in the American Journal of Tropical Medicine and Hygiene. At both hospitals, plasma exchange proved to be a lower-cost, simpler method with fewer side effects than liver transplantation, which was performed on seven patients at HC from January to June 2018, with a success rate of 43%: four died from heavy bleeding, and three survived.
At HC, along with plasma exchange, hemodialysis (filtration of the blood) was also performed intermittently or continuously to compensate for the damage caused to the kidneys by the virus. The medical teams concluded that this procedure should begin when the blood becomes excessively acidic, a condition called metabolic acidosis that is indicated by blood bicarbonate levels falling below normal. In the traditional protocol, hemodialysis was used only when a higher-than-normal level of urea was found.As a supplementary measure, three different types of medication were administered: anticonvulsants to prevent viral damage to the brain, as indicated by levels of ammonia—which is eliminated by the affected liver—rising above normal; antibiotics to fight other infections; and acid reducers. “All patients who underwent these procedures recovered well,” says Ho. As a disease of rapid progression, she says, yellow fever is different from other types of fulminant viral hepatitis and requires continuous monitoring: “Having laboratory tests done twice a day is critical in planning the treatment.”
Ho attributes the reduction in yellow fever mortality this year to yet another change: patients from Vale do Ribeira who presented at the regional hospital in Pariquera-Açu, 220 kilometers from São Paulo City, were promptly sent to HC for treatment on presenting with early signs of the disease—fever, body aches, nausea, and jaundice—without waiting for symptoms to worsen.
Earlier this year, says Ho, physicians involved in the care of yellow fever patients in São Paulo, Rio, and Minas Gerais met to discuss new therapeutic strategies based on the experience of the two hospitals in São Paulo receiving the largest number of cases. Then, at the request of the Pan American Health Organization (PAHO), they submitted to the Ministry of Health a proposed treatment protocol that, if approved, could be adopted countrywide.

Risk indicators
“The epidemic provided a unique opportunity to gain a better understanding of a disease we knew only from sparse case reports,” says epidemiologist Ana Freitas Ribeiro, head of the Epidemiology Service at IIER and a graduate professor at Universidade Nove de Julho (UNINOVE). From January to April 2018, 76 patients with a confirmed diagnosis of yellow fever were admitted at IIER and 97 at HC. The patients were largely from Mairiporã, Atibaia, Cotia, Nazaré Paulista, Guarulhos, and cities in the Baixada Santista area, Registro and São Bernardo do Campo.
In analyzing the cases treated at IIER, Ribeiro and her team found that the condition of patients with yellow fever is more likely to worsen if they have preexisting conditions or an unhealthy lifestyle. “Many were drug users or former drug users,” she noted. Just over half (52%) of patients who died at IIER in 2018 and 27.5% of those who survived consumed alcohol or drugs on a regular basis. Most (80.6%) were men, with an average age of 42 and more than eight years of schooling (55.9%). “The younger the patient and the better their overall health is, the greater their chance of surviving yellow fever,” says Ribeiro. At HC, patients who also had diabetes had a case fatality rate of 80%, as reported in an article in the Journal of Travel Medicine.
Based on their analysis of patients treated last year and this year, the medical teams at HC and IIER have established six indicators for the severity of yellow fever: the levels of aspartate aminotransferase, an enzyme found in the liver; lipase, an enzyme produced by the pancreas; neutrophils, a type of white blood cell; viral load; creatinine, a byproduct of muscle metabolism that is filtered by the kidneys; and coagulation factor V, a protein. These parameters have enabled physicians to screen patients more effectively than before and refer those requiring enhanced care for hospitalization and to ICUs. The new approach is described in detail in papers published in May in Lancet Infectious Diseases, the American Journal of Tropical Medicine and Hygiene, and Memórias do Instituto Oswaldo Cruz.
“These predictors of prognosis, combined with others, provide powerful indicators that can guide decision-making in an ICU setting,” says virologist Pedro Vasconcelos, a researcher at the Evandro Chagas Institute (IEC) in Belém and a professor at the State University of Pará, who was not part of the study. Pathologist Juarez Quaresma, a professor at the Federal University of Pará (UFPA) and a researcher at IEC who was not involved in the recent papers on yellow fever, recognizes the importance of the new indicators but adds: “Future care protocols for critically ill patients should include inflammatory markers, such as interleukin 10 and TNF-α [Tumor Necrosis Factor alpha], which can induce blood vessel damage and contribute to the bleeding seen in severe cases.”
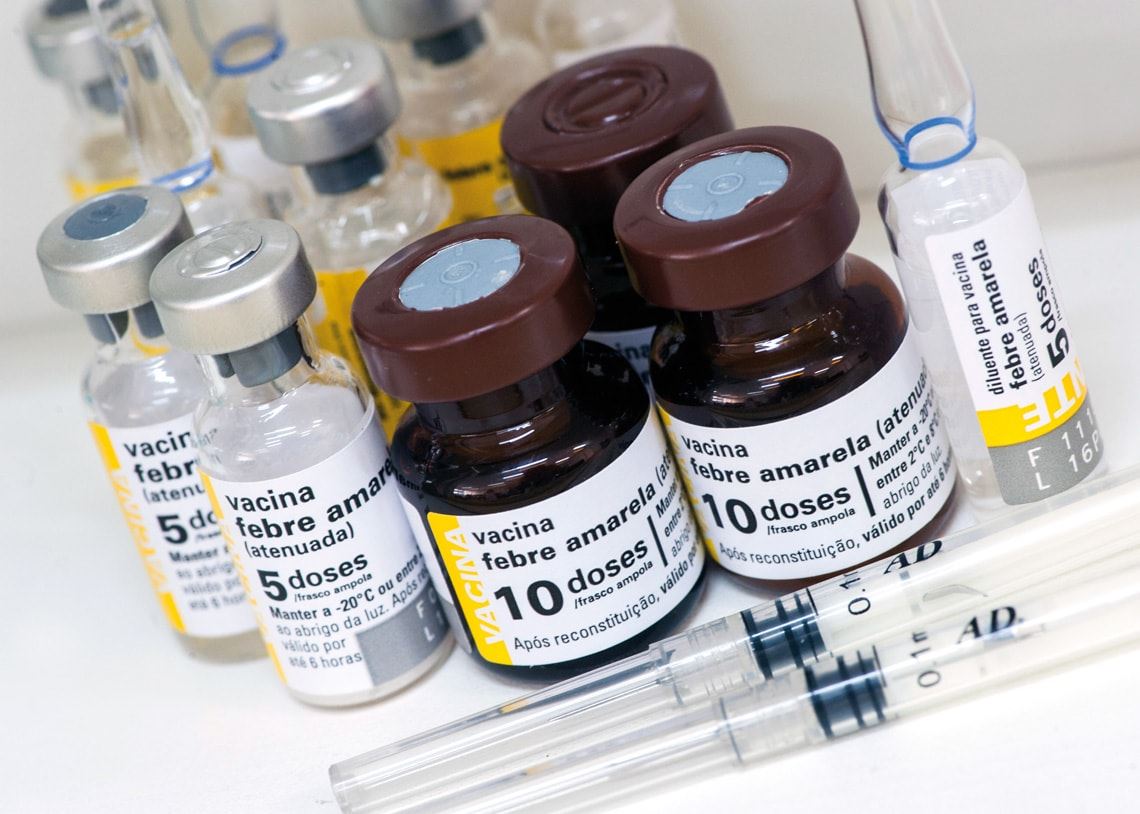
Léo Ramos Chaves
A live attenuated vaccine is the only way to prevent infection with yellow feverLéo Ramos ChavesRecent research indicates that the virus causes more extensive damage to the body than initially thought. In addition to causing direct damage to the liver, spleen, lymph nodes, bone marrow, brain, and heart, as described in recent years, it has now been shown that infection with the virus also facilitates the action of bacteria and promotes the release of toxins that damage the lungs, gut, and pancreas. “The yellow fever virus causes sepsis,” says pathologist Amaro Nunes Duarte-Neto, an assistant physician at USP. He has led 78 autopsies performed on yellow fever patients at the USP Autopsy Service.
The autopsies revealed significant disruption to the body’s defense system. The virus establishes itself in the spleen and lymph nodes, causing a reduction in the population of lymphocytes, a type of white blood cell; in the bone marrow, the disease-causing agent slows the development of these defense cells. In the liver, one of the target organs, “the virus manipulates the immune system and induces the production of anti-inflammatory cytokines that suppress the body’s defenses,” says Duarte-Neto.Autopsies of four people who died after liver transplantation indicated that the virus had migrated from other parts of the body to the engrafted liver, as described in a May article in Histopathology. “The new liver failed to resolve the viral infection in other organs,” he says.
Destruction of the liver undermines the filtration of bacteria and toxins coming from the intestine through the blood, explains Duarte-Neto. These agents find their way directly into the bloodstream and are carried to the rest of the body. Ammonia, one of the byproducts of bacterial metabolism that is no longer retained by the liver, can attack neurons and other cells of the nervous system.
“Alterations in blood microcirculation lead to lung damage and can be induced by both cytokines and secondary bacterial infections,” says Quaresma, based on studies he has conducted at USP and IEC since 2003. “Lung damage is possibly the immediate cause of death for critically ill patients.”
Cases of physicians becoming infected with yellow fever occur as far back as 1685
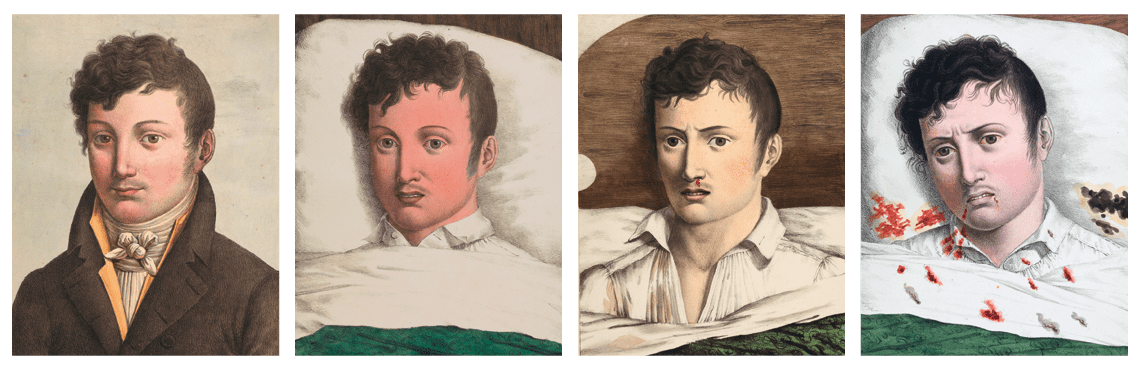
REPRODUCED FROM OBSERVATIONS SUR LA FIÈVRE JAUNE, FAITES À CADIX, 1819 / ETIENNE PARISET AND ANDRÉ MAZET (PARIS, 1820)
An illustration from 1820 depicting the four stages of yellow fever in the same individualREPRODUCED FROM OBSERVATIONS SUR LA FIÈVRE JAUNE, FAITES À CADIX, 1819 / ETIENNE PARISET AND ANDRÉ MAZET (PARIS, 1820)During the first outbreak of yellow fever on record in Brazil, the only physician in Recife, whose name remains unknown, died from the devastating effects of the virus. The outbreak, which struck the capital city of Pernambuco in 1685, led to the death of approximately 600 people during the first weeks. The virus was probably carried by sailors from a ship that had departed from São Tomé, Africa, with a stopover in Saint-Domingue, in the Antilles, where the disease had already spread.
In 1899, during an outbreak that killed 5,000 of Campinas’ 15,000 residents, João Guilherme da Costa Aguiar died at the age of 42. He was one of four physicians who remained in the town to treat the sick; the other 22 had left in the company of wealthy residents fleeing the city.
São Paulo–born oncologist Drauzio Varella contracted yellow fever in 2004 during a field trip to the Rio Negro in the Amazon. Three days after returning to São Paulo, on a Sunday, he began to feel fever, chills, and pain in his back. Colleagues admitted him to the hospital, and successive blood tests indicated severe hepatitis and a diagnosis of yellow fever. That year, the Brazilian Ministry of Health recorded only five cases of yellow fever, with three deaths.
“He had hepatic coma, was very ill and thought he was going to die,” recalls Kallas, who led the medical team alongside hepatologist Flair Carrilho, a professor at FM-USP. At age 61, Varella had pneumonia in both lungs, kidney failure, and a decrease in coagulation factors but no bleeding.
Blood tests showed a slow recovery over the space of several months. Kallas attributed Varella’s recovery first to luck: “Everyone who treated him was very dedicated and collaborative.” In addition, Varella’s healthy lifestyle, which included regular jogging—on the Sunday before his hospitalization, he had run 18 kilometers and climbed the stairwell of his 14-floor apartment building—contributed to his good fortune. “If he had other preexisting conditions,” says Kallas, “his recovery would certainly have been much more difficult.”
Varella recognized that it had been a mistake to not take a booster dose of the yellow fever vaccine before traveling to the Amazon, an area with a high risk for transmission of the virus. He described his ordeal in the book O médico doente (The sick physician; Companhia das Letras, 2007).
Projects
1. Viral metagenomics to track, explain, and predict the transmission and spatiotemporal spread of Dengue and Chikungunya viruses in Brazil (nº 16/01735-2); Grant Mechanism Regular Research Grant; Principal Investigator Ester Cerdeira Sabino (USP); Investment R$445,187.99.
2. Genetic and phylodynamic diversity of emerging and re-emerging arboviruses (DENV, ZIKV and CHIKV) in the Northeast and Southeast regions of Brazil, 2014–2016 (nº 16/08204-2); Grant Mechanism PhD Grant; Principal Investigator Paolo Marinho de Andrade Zanotto (USP); Scholarship Beneficiary Marielton dos Passos Cunha; Investment R$148,954.26.
Scientific articles
RIBEIRO, A. F. et al. Yellow Fever: Factors associated with death in a hospital of reference in infectious diseases, São Paulo, Brazil, 2018. American Journal of Tropical Medicine and Hygiene. May 28, 2019.
DUARTE-NETO, A. N. et al. Yellow fever and orthotopic liver transplantation: New insights from the autopsy room for an old but reemerging disease. Histopathology. May 14, 2019.
HO Y. L. et al. Severe yellow fever in Brazil: Clinical characteristics and management. Journal of Travel Medicine. Online. May 31, 2019.
Published in September 2019
Republish