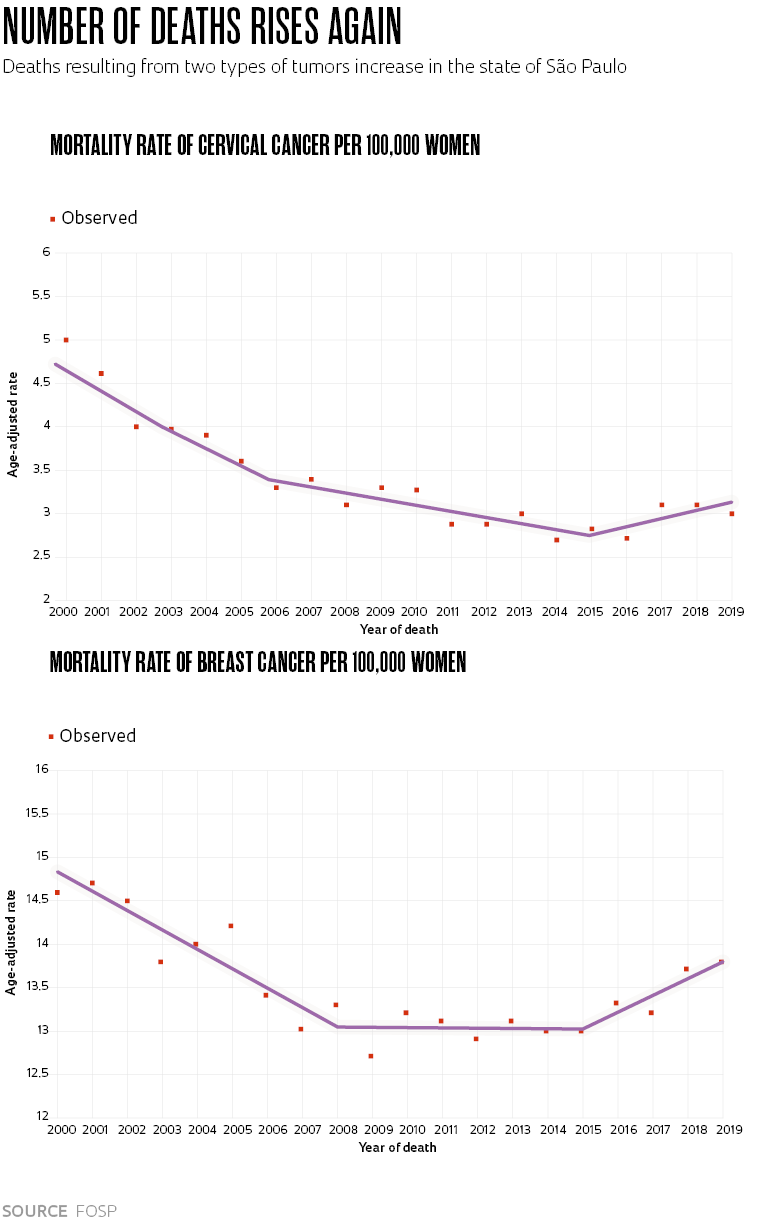
On the computers of the Information and Epidemiology unit at the Oncocentro Foundation of São Paulo (FOSP), two graphs are seen with surprise and apprehension. They indicate increased mortality rates in the state of São Paulo for breast and cervical cancer since the middle of the last decade. It is the first time, since the start of the 2000s, that these figures have shown an upward trend.
Deaths from these types of tumors had fallen consistently until 2008, followed by a period of less intense reduction in the case of cervical cancer and of stability for breast cancer. Until, in 2016, the deaths started increasing again. In 2019, the last year with analyzed data, for every 100,000 women there were 3.2 deaths from cervical cancer and 13.8 for breast cancer in the state of São Paulo. At the best moment, the fatality rates of these two tumors were 2.8 and 13 deaths per 100,000 women, respectively.
“São Paulo is the first Brazilian state to show a reverse trend in mortality for cervical cancer,” says epidemiologist Carolina Luizaga, of FOSP, the support agency for cancer policies of the São Paulo State Health Department that records the cases of the disease, does research, and aids in training of specialized workers in the area. Luizaga recently completed a study, about to be published, on the evolution of this disease in the Southeast region of Brazil. The work draws attention to the increased risk of death from this type of tumor among younger women, in the age range from 25 to 39 years old. Preliminary data about breast cancer, also in the Southeast, similarly signal an increase of 1.48% in its lethality each year, between 2015 and 2019.
In Brazil, it is breast cancer that affects and kills the most women. Cervical cancer is third for incidence and fourth for deaths among the country’s female population. This year, according to estimates from the National Cancer Institute (INCA), 66,000 new cases of breast cancer (almost 30% of all tumors diagnosed in women) and around 17,000 deaths (16.5% of female deaths from neoplasms) are expected. The incidence and mortality rates for cervical cancer are equivalent to approximately one-quarter and one-third, respectively, of the numbers associated with breast tumors.
The factors that have changed the epidemiological situation of these two types of cancer in women in São Paulo still need to be studied further. For now, there are some hypotheses that attempt to explain the phenomenon, also recently found in developed countries. According to Luizaga, the increased death rate for cervical cancer among younger women could be related to changes in their sexual behavior. They are becoming infected more frequently by human papillomavirus (HPV), which can be transmitted during sexual intercourse and the presence of HPV increases the incidence of cervical cancer—although it is possible to prevent the problem. A vaccine against this virus is now available in the public health system, aimed at boys and girls aged from 9 to 14 years. “Besides this, younger women are integrated into the economically active population, they work and have less free time. This can complicate adhesion to screening,” says the epidemiologist.
Screening is the key word in the assessment of physician Victor Wünsch Filho, professor at the School of Public Health of the University of São Paulo (FSP-USP) and chairman of FOSP. For him, the rising trend in the mortality curves likely results from failures in current screening and early diagnostic practices, meaning in the procedures that enable the discovery of precancerous lesions and early-stage cancer. “The structure needs to be changed. It is necessary to implement organized population-based screening,” defends the physician, who has just started a project about controlling cancer in the state of São Paulo within the scope of the Science Centers for Development initiative, created this year by FAPESP.
Wünsch explains that opportunistic screening is the predominant type in the country, which occurs when women look for health facilities for any type of consultation and take the opportunity to carry out preventive gynecological exams. The number of these procedures has reduced. “Between 2009 and 2020 drops were observed in the percentages of cover for cytology tests, also called Papanicolaou tests, especially among younger women,” comments the physician. The Papanicolaou test aims to identify the early appearance of cervical lesions.
The director of FOSP advocates that the state of São Paulo implements organized screening, actively seeking women from the target age range to take the exams and monitor the results. “We don’t have this monitoring today. It is necessary to guarantee that women from the target audience have the tests and then those who receive results with alterations follow the line of care. It has already been verified that 35% of women are ‘lost’ in the system,” warns the director.
A study published last year in the journal Cancer Epidemiology analyzed the records of 4,300 women over the age of 25 from the state of São Paulo who were examined in 2010 and had a high-grade lesion—a precursor of cervical cancer—detected by the cytology test. According to the work, approximately one in every three patients that received this diagnosis did not appear for further investigation in the three years following the exam. “The basic health units are often unable to track the altered cases to carry out additional exams and treatment,” evaluates the technical department manager of FOSP, Lise Balter Cury, one of the authors of the study.
Another alarming piece of information from the research was the average time spent between suspicion (during screening) and confirmation of the diagnosis: 190 days. This is the overall average for the state of São Paulo, with local variations: 198 days in the state capital, 274 in the Metropolitan Region (excluding the capital city), and 149 days in the interior of the state. The average time between confirmation of the diagnosis and initiating treatment was 81 days in the state of São Paulo. In the state capital, this number was 98 days, 103 in the Metropolitan Region, and 57 days in the interior. In this scenario, only the service in the interior of São Paulo State was compatible with Federal Law No. 12.732/2012, also known as the “60-day Law,” according to which all persons diagnosed with cancer must receive treatment within 60 days after confirmation of the diagnosis.
The delay in starting oncology treatment does not only occur in poor or middle-income countries. According to a study coordinated by mastologist César Caello, of the School of Medical Sciences at the University of Campinas (FCM-UNICAMP), the problem also exists in the US health system. In an article published at the beginning of this year in the scientific journal Oncologist, he compared the attendance of patients with breast cancer in three public hospitals in São Paulo and Rio de Janeiro, and two from the state of Texas, in the USA. The average time taken between diagnosis and the first treatment was very close in the two countries: 9.9 weeks in Rio de Janeiro and São Paulo, and 9.4 weeks in Texas. Data from 1,191 women (963 from Brazil and 228 from the USA) diagnosed between 2009 and 2011 were investigated.
The key to understanding this phenomenon appears to be in the disorganization of the public health systems, which causes delays in screening, diagnosis, and starting treatment. “In the USA, organized screening is linked to health insurance, it doesn’t exist in public healthcare,” explains Cabello. “For this reason, patients from lower socioeconomic levels, who cannot afford insurance and use hospitals in the US public system, can have delays similar to those faced by Brazilians.”

Eter Dazeley / Getty ImagesPapanicolaou testEter Dazeley / Getty Images
The impact of the pandemic
The overloading of public health services and the social-distancing measures caused by the Covid-19 pandemic made it difficult to control and fight cancer. Measuring this impact on the diagnosis of the main tumors that affect women was the objective of a study carried out at UNICAMP and the Federal University of Uberlândia (UFU). The researchers analyzed the number of mammograms, conizations (cervical biopsies) and Papanicolaou tests done in the state of São Paulo between January 2017 and November 2021. During the pandemic, around 1.9 million fewer exams and procedures were carried out than forecast and there was a reduction of 25% in the initiation rate of treatment for breast cancer in the initial stages.
A worrying number also emerged for cervical cancer: 156 more cases were diagnosed, compared with the average from the pre-pandemic period, of patients in an advanced stage of the disease with little chance of being cured and immediately referred to the palliative care sector. “The impact of delayed screening is noticed over a longer period, but the damage of delayed diagnosis is immediate,” warns oncologist José Barreto Carvalheira, of UNICAMP, one of the authors of the study.
The Oncocentro Foundation is the largest public laboratory specialized in cancer in the country. It provides services for 546 health units from 56 municipalities. The impact of the pandemic on the quantity of exams carried out is also evident in FOSP, but the situation is already improving. “In 2019, for example, we performed 246,000 cytology tests for cervical cancer screening. At the height of the pandemic, in 2020, this number fell to 130,000. We expect to close 2022 having carried out around 200,000 cytology tests. A slow recovery is happening,” highlights pathologist Alexandre Ab’Saber, technical director of FOSP.
José Carvalheira estimates that the countries with organized screening will return to normality much quicker. He cites England as an example: “There, patients receive a letter at home inviting them to carry out the exams; here, the exams are sporadic,” he compares. Before the pandemic, the World Health Organization (WHO) had global targets to reduce the death rates for cervical and breast cancer by 30% and 25%, respectively, by 2030. With the outbreak of Covid-19, the objectives have become more difficult to achieve.
Project
Control of cancer in the state of São Paulo (ConeCta-SP): From knowledge to action (nº 21/11794-4); Grant Mechanism Research Grant – Science Centers for Development; Principal Investigator Victor Wünsch Filho (FOSP); Investment R$1,299,390.51.
Scientific articles
RIBEIRO, C. M. et al. Follow-up of women screened for cervical cancer in São Paulo, Brazil: An analysis of the times to diagnostic investigation and treatment. Cancer Epidemiology. april 24, 2021.
SHAFAEE, M. N. et al. Breast cancer treatment delay in SafetyNet Health Systems, Houston versus Southeast Brazil. Oncologist. march 28, 2022.
Republish