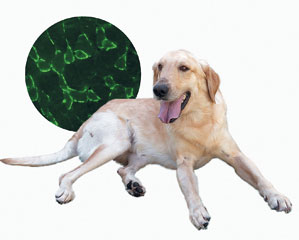
Eduardo Cesar (dog) and Natássia Vieira Cells (detail) produce human dystrophin in dogs and rodentsEduardo Cesar (dog) and Natássia Vieira
With its front legs hanging on to a miniature bar the mouse raises its body until its back legs also hang on to the wire, thus preventing it from falling. This small acrobat is the most recent hope for the group working with geneticist, Mayana Zatz, from the Center for Human Genome Studies at the University of São Paulo (USP), one of the Research, Innovation and Dissemination Centers financed by FAPESP to fight muscular dystrophy, a genetic disorder that affects 1 in every 2,000 Brazilians. Although there is no cure for muscular dystrophy, starting in infancy it causes the progressive degeneration of the muscles leading to a loss of movement and the need for apparatus to help with breathing.
Over the last few years Mayana’s team has been testing different types of adult stem cells, extracted from the fat discarded following liposuction, from milk teeth and from the umbilical cord, on animal models that develop a problem similar to human muscular dystrophy.
In the case of the acrobatic mouse stem cells from human fat complemented its versatility and were transformed into muscle. The team from USP used 21 mice, divided into three groups. One of them received undifferentiated stem cells that were not manipulated after they were extracted from the human body. Cells that were a little more mature and that had been treated in the laboratory to become muscle cells were injected into the second group. The third group received no treatment and served for comparison purposes with the other two.
The result was surprising. According to data published in the journal, Stem Cells, the most marked improvement was in animals treated with undifferentiated cells. “It seems as though the cells develop better in the organism than in the laboratory”, comments Mayana.
The effect of the treatment can be seen even by those who are not researchers. The mice from the control group (untreated) remained almost a minute hanging on the bar before falling. Those that received the injection of stem cells did well in the test – these animals had an average increase in muscular strength of 15%.
There are reservations, however, as to the use of mice as a model for investigating human muscular dystrophy. Mutations in the gene that produces dystrophin, the protein responsible for most of the cases of the disease in human beings, do not cause a visible weakness in rodents. Because of this, in the tests the team from USP used mice with muscular dystrophy caused by a deficiency in the production of the dysferlin protein, which causes the most visible symptoms of the human disease in animals. The improvement was not just clinical: “Human stem cells were transformed into muscle and started producing all the muscular proteins, including dysferlin and dystrophin”, says geneticist Natássia Vieira, the work’s main author. This is an indication that human proteins also fulfill their function in other mammals.
Mayana’s team is trying to overcome the restrictions of carrying out studies on mice by working in partnership with Maria Angélica Miglino’s group, from USP’s School of Veterinary Medicine, with golden retriever dogs. These animals have signs of dystrophy that are closer to those of children who seek help at the Center for Human Genome Studies. But not everything is perfect: dogs take up more space, eat more food and do not reproduce as quickly as rodents, which is why working with them is slower.
The most recent advance in the treatment of dogs is already available on the website of the Journal of Translational Medicine. Headed up by geneticist Irina Kerkis, from the Butantan Institute and by veterinarian Carlos Ambrosio, from USP, the group compared the effect of two different ways of applying the stem cells: directly into the muscle or into the blood stream. Irina and Ambrosio injected stem cells taken from human milk teeth into four golden retriever pups, two male and two female, and saw that the cells injected into the blood have more chance of being incorporated into the muscle of the affected animal.
Mayana is not yet celebrating the result. Of the four animals treated only a male is still alive and healthy after the end of the study. “He may only be alive because he’s a relative of Ringo”, reflects the geneticist, referring to the dog that at 5 years old has no symptoms of the disease despite having it genetically. Discovering why may change the way of fighting muscular dystrophy.
Republish