Washing hands, cutting hair short, drinking filtered water and boiled milk, maintaining a clean home, and other daily habits come from the ideas promoted by the French chemist, Louis Pasteur, surrounding disease transmission by microorganisms in the late nineteenth century. He was born 200 years ago, in December of 1822, in Dôle, a city in eastern France. Upon his death in 1895, at the age of 72, he had become one of the most important characters in the history of global science—and even today he is the namesake of streets, schools, buildings, research centers, and clinical analysis laboratories. The Pasteur Institute in Paris is one of the planet’s largest research institutions dedicated to infectious diseases and vaccine production, with branches in 26 countries.

Instituto Pasteur / Museu PasteurThe Angel of Inoculation, a cartoon by Charles Gilbert-Martin published in 1886Instituto Pasteur / Museu Pasteur
During the second half of the nineteenth century, alongside German pathologist Robert Koch (1843–1910), Pasteur laid the foundations of microbiology and the—now obvious—concept that infectious diseases are caused by microorganisms and can be prevented through hygiene measures and vaccines. “Our minds became Pasteurian,” summarizes science historian Jaime Benchimol, of the Oswaldo Cruz Foundation’s Oswaldo Cruz House (COC-FIOCRUZ) and author of the book Febre amarela: A doença e a vacina, uma história inacabada (Yellow fever: The disease and the vaccine, an unfinished story; Editora Fiocruz, 2001). English physician Joseph Lister (1827–1912) visited Pasteur in 1876 in Paris and based on his French colleague’s ideas, decided to disinfect surgical instruments and the surgical site, thus reducing infections.
Pasteur broke down the barriers separating basic and applied science by stating that there was no applied science, but applications of science. In the book Pasteur’s Quadrant: Basic Science and Technological Innovation (Brookings Institution Press, 1997), North American political scientist Donald Stokes (1927–1997) used two axes to classify research activities—the vertical, representing the capacity to generate basic knowledge, and the horizontal, reflecting the applications.
From there, four quadrants emerge: at the bottom, closest to where the two axes meet, the quadrant remains blank; alongside the blank quadrant, to the right, is the Thomas Edison (1847–1931) quadrant, alluding to the North American inventor who created the incandescent light bulb and who is highly relevant to applications and hardly relevant to knowledge; on top, to the left, is the Niels Bohr (1885–1962) quadrant, referring to the Danish physicist who enabled major advancements in the structure of the atom; and on top, to the right, the Pasteur quadrant, for the chemist who reconciles advancements in both knowledge and applications.
Stokes argued that the French chemist had two commitments: “understanding the microbiological processes that he discovered” while simultaneously “controlling the effects of such processes on various products and on animals and human beings alike.” Thus, the author shows that so-called basic or fundamental science can generate economic or social gains. This idea contradicts the separation between pure science and applied science, strengthened after the Second World War, which influenced science and technology policy in the following decades (see Pesquisa FAPESP issue no. 110).
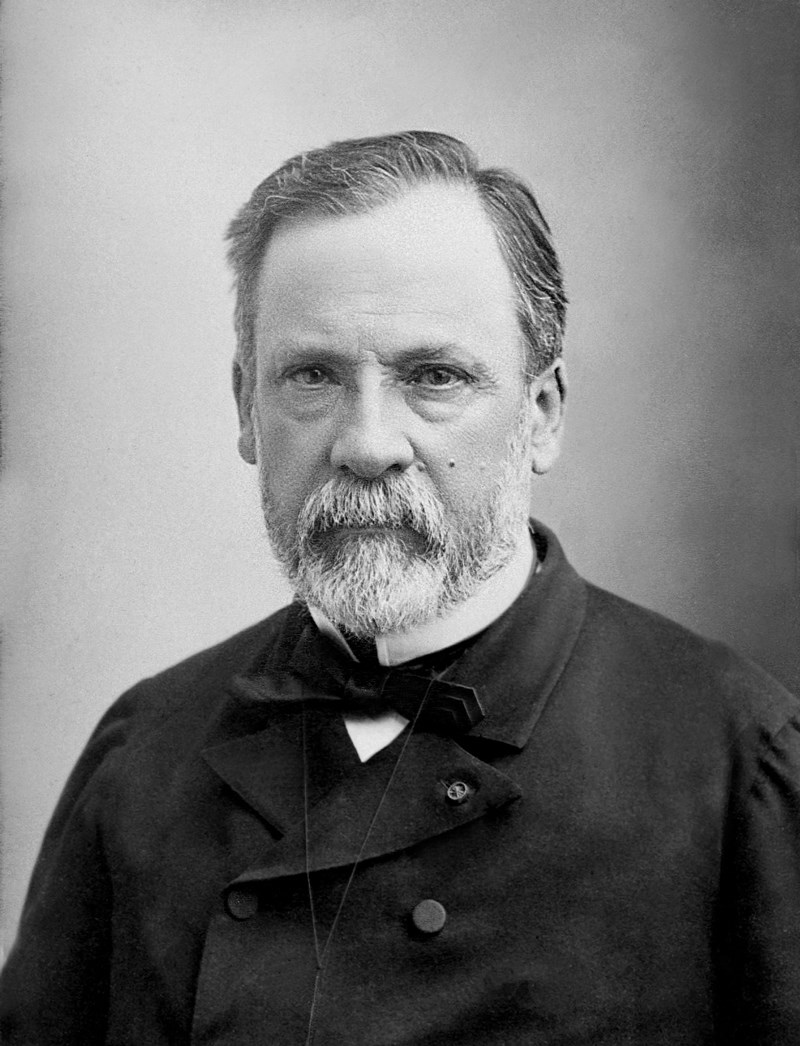
Wellcome LibraryPortrait of the French chemist by Félix Nadar in 1878Wellcome Library
Vaccines
Along with his team, he was one of the first to produce science-based vaccines in a laboratory for veterinary and human use against infectious diseases. The first vaccine was for a disease called “anthrax” that was afflicting sheep. It is caused by the bacterium Bacillus anthracis, identified by Koch in 1877. Confident in his experience working with animals in the lab, Pasteur held a public exhibition, in June of 1881, in the town of Pouilly-le-Fort, southeast of Paris, before veterinarians, farmers, local politicians, and reporters. With his assistant, chemist Charles Chamberland (1851–1908), he showcased the vaccine he had developed, which uses an attenuated version of the bacteria that causes the disease, administering it to 25 sheep, while leaving 25 others unvaccinated. Next, he injected all the sheep with a solution containing the bacteria. Twenty-four of the vaccinated sheep survived, while the others died.
In 1857, after teaching chemistry for three years at the University of Lille, he began lecturing at the Normal Superior School in Paris. In 1889, he decided to dedicate himself to vaccines for human use. He began with rabies, a viral disease transmitted mainly through the saliva of infected animals.
In July of 1885, he treated a 9-year-old boy, Joseph Meister (1876–1940), whose arms and legs had been bitten by a rabid dog. He himself reported: “The child’s death appeared inevitable. I decided, not without deep anguish and anxiety, as one can imagine, to apply to Joseph Meister the method which I had tried with consistent success in dogs.” It worked, and the boy recovered after 13 injections.
After examining Pasteur’s laboratory notebooks, North American historian Gerald Geison (1943–2001) argues in the book The Private Science of Louis Pasteur (Princeton University Press, 2014) that Joseph Meister was not the first to receive the rabies vaccine. Secretly, Pasteur had already used it on a 61-year-old man named Girard, who survived, and an 11-year-old girl, who died. The notes “reveal that Girard was injected with a formula that Pasteur had not described in writing—namely, an emulsion of the spinal cord of a rabbit killed by hydrophobia experiments, which had been left to dry in a hermetically sealed flask for about two weeks,” reports Geison.
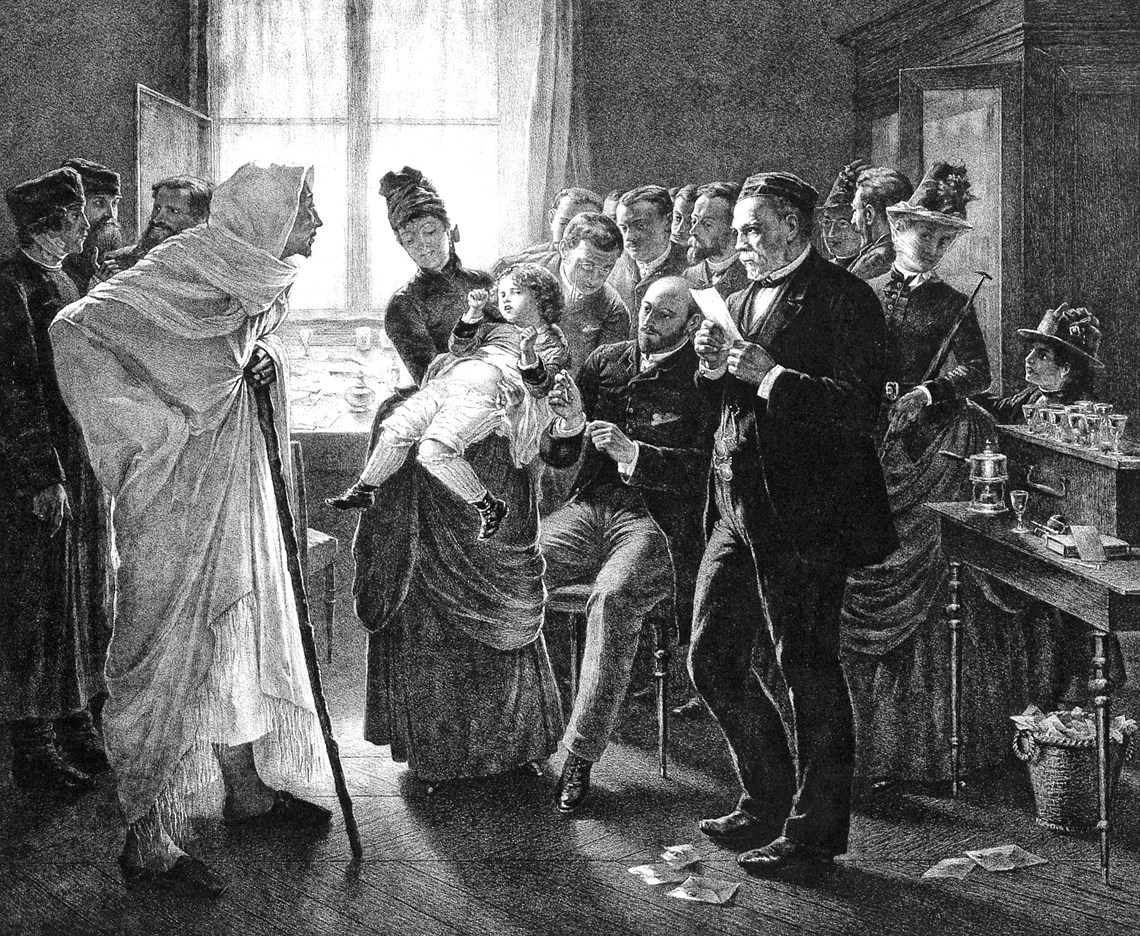
Wellcome Library, London. WellcomeLithograph of a rabies vaccination clinic in ParisWellcome Library, London. Wellcome
According to him, the French chemist had not yet tried to cure rabies in animals before treating Girard. “The notebooks do not provide any proof that Pasteur had conducted the experiments on animals, which he used to justify his decision to treat Meister,” adds the historian. When he treated the young boy, he had only begun an experiment involving 40 dogs, with various formulas, and the results were not yet comparable. Even so, Pasteur carried on because he was moved by the boy’s situation. The boy would go on to work at the Pasteur Institute until the Nazi Army entered Paris in 1940 and he ended his own life.
During a conference at the French Academy of Sciences in Paris, in March of 1886, the chemist proposed creating an institute to produce and administer the rabies vaccine, based on his findings. With the Academy’s support, donations flooded in from everywhere, including from the Emperor of Brazil, Dom Pedro II (1825–1891).
“Dom Pedro II was already particularly interested in the sciences when he met Pasteur,” recounts chemist and science historian Carlos Alberto Lombardi Filgueiras, of the Federal University of Minas Gerais and author of the book As origens da química no Brasil (The origins of chemistry in Brazil; Editora UNICAMP, 2015). “He became fascinated with what, at the time, was known as bacteriology, now known as microbiology, and made a point of donating his own money to build the Pasteur Institute in Paris.”

O Album, year 1, no. 22. 1893Domingos José Freire, recommended by the French chemist to fight yellow fever in BrazilO Album, year 1, no. 22. 1893
Filgueiras discovered a letter in the archive at the Imperial Museum of Petrópolis, in Rio de Janeiro, in which Pasteur responded to an invitation from the emperor to come to Rio de Janeiro and research yellow fever, which was the cause of an epidemic in Brazil at the time. He apologized for fearing the effects of a tropical climate at the age of 62, claiming he had to dedicate himself to the rabies vaccine and recommending the Rio de Janeiro–based physician, Domingos José Freire (1843–1899), who had created and administered an experimental yellow fever vaccine (see Pesquisa FAPESP issue no. 265).
The emperor also supported the Pasteur Institute in Rio de Janeiro, linked to the Santa Casa da Misericórdia and inaugurated in February of 1888, nine months prior to the Pasteur Institute in Paris. “Our medical elite was extremely well-informed and well-educated over there,” explains historian Luiz Antonio Teixeira, also of COC-FIOCRUZ, while explaining how quickly the techniques for producing anti-rabies serum were incorporated. In Recife (Pernambuco), an anti-rabies institute was founded and named after the French chemist the following year; in the city of São Paulo, in 1903; in Juiz de Fora (Minas Gerais), in 1908; in Porto Alegre (Rio Grande do Sul), in 1910; and in Florianópolis (Santa Catarina), two years later.
“Generally speaking, the institutes in Brazil and in other countries were created merely to reproduce the technique used to produce the rabies vaccine,” says Teixeira, author of the book Ciência e saúde na terra dos bandeirantes: A trajetória do Instituto Pasteur de São Paulo no período de 1903-1916 (Science and health in the land of the pioneers: The trajectory of the Pasteur Institute in São Paulo from 1903–1916; Editora FIOCRUZ, 1995). “The one in São Paulo was the only institute also dedicated to scientific research because it had already started a network of health institutes, such as the bacteriological and the vaccinogenic institutes” (see Pesquisa FAPESP issue no. 300). Created as a private institution by a group of physicians, the São Paulo institute, due to financial struggles, was donated to the state government in 1916. Those in other states were incorporated by health agencies or closed after rabies outbreaks disappeared. Today, the disease is quite rare and is transmitted mainly by common vampire bats.

Wikimedia CommonsPasteur working on an experiment in his laboratoryWikimedia Commons
“Many physicians from Rio de Janeiro [Brazil’s capital at the time] swiftly embraced the germ theory proposed by Pasteur, but there was also quite a bit of controversy, because the new ideas contradicted established beliefs, such as the belief that diseases resulted only from unhealthy environments,” says Benchimol. “Bacteriology was born amid suspicion and doubt.” Between 1878 and 1886, the Medical Gazette of Bahia (GMBahia) published translations of Pasteur’s articles about the applications of the germ theory in medicine that allowed for more extensive and safer surgeries with a lower risk of infection, and about tests using the rabies vaccine, but the newspaper also allowed room for opposing views to be expressed.
“Bacteriology had a major impact on collective health, because it enabled the prevention of infectious diseases, through patient isolation, vaccination, and the population’s improved living conditions in order to avoid transmitting pathogens,” comments Teixeira. It was based on Pasteur’s ideas that the physician Oswaldo Cruz (1872–1917) quelled the yellow fever epidemic at the start of the twentieth century.
According to Teixeira, one of bacteriology’s limitations is what he calls “unicausality”—identifying a single cause for the emergence of a disease or epidemic, which overshadows the existence of other factors, such as living conditions, which favor the evolution of diseases, like tuberculosis: “For decades, the unicausal view of diseases limited public health actions.” The situation began to change in Brazil starting in the 1920s, mainly with the appearance of pharmacist and physician Geraldo Paula Souza (1889–1951).

Museu Pasteur / Instituto PasteurOfficial delegation in front of the Notre-Dame cathedral at his funeral on October 5, 1895Museu Pasteur / Instituto Pasteur
Professor at the University of São Paulo’s School of Medicine (FMUSP) and founder of the Institute of Hygiene, which would become the University of São Paulo’s School of Public Health (FSP-USP), Paula Souza had a broad view of health issues, not merely biological, and created a network of health clinics that combined prevention with health education, based on what he had seen in the United States. In 1945, he participated in the San Francisco Conference, in the United States, which led to the creation of the United Nations (UN) and supported the formation of the World Health Organization (WHO), three years later.
Republish