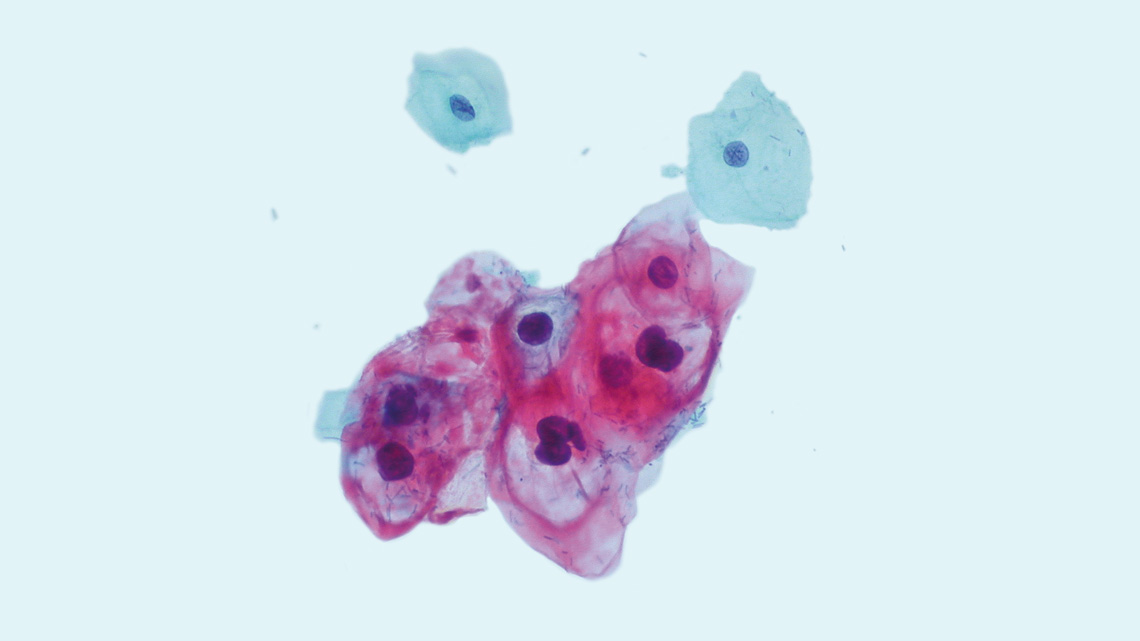
A vaccine that can treat certain types of viral cancer, rather than solely preventing the underlying viral infection, could be on its way to the market. In a study published in March in Science Translational Medicine, researchers from the University of Pennsylvania and the University of São Paulo (USP), Brazil, reported encouraging results from animal tests of a candidate vaccine designed to combat tumors caused by chronic HPV infection. HPV is a virus transmitted through sexual contact that is responsible for several common forms of cancer, including cervical cancer.
The new vaccine employs the same messenger RNA (mRNA) technology used by Pfizer/BioNTech in the production of COVID-19 vaccines, and similarly belongs to the category of therapeutic agents. The vaccine works by stimulating the immune system to eliminate already diseased cells, rather than preventing HPV infection like other vaccines currently available in most countries.
In experiments with mice, a single dose of the new candidate eradicated tumors in different regions of the body, even in advanced stages. Although the results are promising, it will still take some time for the formulation to become available for use in humans.
During her doctoral studies under microbiologist Luís Carlos de Souza Ferreira at USP, biotechnologist Jamile Ramos da Silva completed a research fellowship as part of a group led by Hungarian biochemist Norbert Pardi at the University of Pennsylvania, where she helped to develop three formulations that utilize mRNA molecules to teach the immune system to recognize and attack HPV-infected cells.
One of the formulations administered to mice employed an RNA molecule in its naturally occurring form, composed of a sequence of nitrogenous bases: adenine (A), cytosine (C), guanine (G), and uracil (U). This RNA molecule was incapable of spontaneous replication within cells. Referred to as unmodified nonreplicating RNA, this version typically induces a more intense inflammation response, which is desirable for combating tumor cells. However, excessive inflammation can be potentially fatal as it affects the entire organism. The second version of the vaccine candidate utilized a modified nonreplicating RNA molecule, developed with the same strategy as used for some COVID-19 vaccines. In this version, uracil was replaced with a synthetic molecule that helps to reduce inflammation. The third formulation was based on RNA containing a special segment that enables self-replication within cells. This mechanism allows for increased synthesis of proteins that activate defense cells against tumors using lower concentrations of genetic material.
In all formulations, the RNA molecule contained instructions for making two proteins: E7 from HPV, which remains exposed on the surface of tumor cells infected by the virus, and glycoprotein D, which is contained in the outer layer of the herpes virus. “The first protein signals the immune system to target and destroy specific cells, while the second protein enhances the immune response,” explains Ferreira, one of the lead authors of the study.
Encased in a lipid layer that protects them from degradation before entering cells, the RNA molecules carrying the instructions for these two proteins were tested at four different dosages. Each dosage was administered through a single intramuscular injection, targeting tumors of various sizes and locations.
In one experiment conducted at the Vaccine Development Laboratory of the Institute of Biosciences at USP, Ramos da Silva implanted tumor cells beneath the skin of mice and divided them into three groups: one group received an injection of the formulation containing unmodified nonreplicating RNA, another group received the modified nonreplicating RNA, and a third group received the self-replicating RNA.
All three versions prevented cancer development, but the latter two proved to be more effective. All animals treated with the vaccine based on modified RNA or self-replicating RNA remained completely tumor-free throughout the 70-day follow-up period (a mouse typically lives around a thousand days). Among those that received the unmodified RNA, the survival rate was 80%. In the control group, which received an inert compound (placebo), all subjects developed cancer and had to be euthanized within one month. Analyses showed that these RNA-based formulations activate CD8 T lymphocytes, which recognize HPV-infected tumor cells and destroy them by perforating their membranes.
In a test simulating cancer recurrence, which is common in many types of cancer, Ramos da Silva reimplanted tumor cells in the mice 90 days after the vaccine dose. Once again, the formulations based on modified RNA and self-replicating RNA prevented recurrence, while immunization with unmodified nonreplicating RNA protected only half of them. When tumors were implanted in other regions of the body, such as the vagina or tongue, mimicking sites where HPV-related cancers occur, the unmodified RNA and self-replicating RNA formulation performed better and resulted in regression in 100% of cases. These data were reported in a paper in Science Translational Medicine and were presented by Ramos da Silva at the annual meeting of the American Association for the Advancement of Science (AAAS) held March 2 in Washington, DC.
Even against advanced-stage disease, the RNA-based vaccine candidates performed remarkably well with just a single injection, allowing 60% of the animals to become and remain completely cancer-free for an extended period of time.
All RNA-based formulations yielded significantly superior results compared to two other vaccine technologies the researchers evaluated: one using a DNA molecule coding for E7 and glycoprotein D, and another where a hybrid molecule purified from the two proteins was directly administered to the animals. “The RNA-based formulations, even at very low doses, demonstrated unparalleled effectiveness,” says Ferreira.
Despite the encouraging results, it will still take several years before a therapeutic vaccine is available to the general population. Before this happens, additional animal experiments are required to assess the formulations’ efficacy and safety, and to ensure they are produced in accordance with good manufacturing practices mandated by regulatory agencies.
But the effort will be worthwhile. “Developing an effective therapeutic vaccine against tumors caused by HPV would be groundbreaking for the treatment of genital organ cancers, especially advanced-stage cervical cancer, a field that has seen little progress in the past 20 years,” says oncologist Glauco Baiocchi, director of the Department of Gynecologic Oncology at A.C.Camargo Cancer Center in São Paulo. In approximately 95% of cases, this type of tumor is associated with HPV infection and is commonly treated with a combination of surgery and radiotherapy.
The two currently available vaccines—Gardasil, produced by Merck, and Cervarix, produced by GlaxoSmithKline—are effective but only prophylactic. These vaccines stimulate the production of antibodies that bind to the virus, preventing its entry into cells and thereby reducing the risk of developing genital (cervical, vaginal, penile, and anal) or head and neck (mouth and throat) cancers. “These vaccines can prevent almost 100% of these tumors, but only in individuals who have not had prior exposure to HPV,” explains Baiocchi. For this reason, they are administered to children and adolescents prior to the onset of sexual activity.
Projects
1. Discovery of antigens and development of serological diagnostic methods and vaccine strategies for the Zika virus (ZIKV) (nº 16/20045-7); Grant Mechanism Thematic Project; Principal Investigator Luís Carlos de Souza Ferreira (USP); Investment R$958,175.01.
2. Targeting antigens at dendritic cells as a strategy for improving the efficiency of immunotherapies for HPV-16-associated tumors (nº 18/26515-0); Grant Mechanism Regular Research Grant; Principal Investigator Luís Carlos de Souza Ferreira (USP); Investment R$216,944.50.
3. Self-amplifying RNA vaccine as an immunotherapeutic strategy for controlling HPV-16-induced tumors (nº 16/11594-7); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Jamile Ramos da Silva; Investment R$321,885.68.
4. RNA vaccines for HPV-induced tumors (nº 19/01523-3); Grant Mechanism Doctoral Fellowship Abroad; Principal Investigator Luís Carlos de Souza Ferreira (USP); Beneficiary Jamile Ramos da Silva; Supervisor Norbert Pardi (University of Pennsylvania); Investment R$80,892.33.
5. Controlling HPV-induced tumors with immunotherapy based on the association of monoclonal antibodies that block immunosuppressive pathways and a therapeutic vaccine capable of activating cytotoxic CD8+ T lymphocytes (nº 16/14344-1); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Natiely Silva Sales; Investment R$226,459.68.
6. Targeting antigens at dendritic cells as an immunotherapeutic strategy for controlling HPV-associated tumors (nº 18/07629-5); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Mariângela de Oliveira Silva; Investment R$187,218.60
7. New therapeutic frontiers against tumors caused by the human papilloma virus (HPV): experimental evaluation of the association of chemotherapy and vaccine strategies (nº 13/15360-2); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Luana Raposo de Melo Moraes Aps; Investment R$215,707.18.
8. Active immunotherapy based on dendritic cells combined with chemotherapy to treat advanced stage HPV-16-associated tumors (nº 21/03326-0); Grant Mechanism Doctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Karine Bitencourt Rodrigues; Investment R$101,287.44.
9. Human papillomavirus (HPV)–induced neoplasms: A new therapeutic approach based on active immunotherapy by targeted stimulation of dendritic cells (nº 17/21358-1); Grant Mechanism Postdoctoral Fellowship in Brazil; Supervisor Luís Carlos de Souza Ferreira (USP); Beneficiary Bruna Felício Milazzotto Maldonado Porchia Ribeiro; Investment R$350,326.41.
Scientific article
RAMOS DA SILVA, J. et al. Single immunizations of self-amplifying or nonreplicating mRNA-LNP vaccines control HPV-associated tumors in mice. Science Translational Medicine. Mar. 3, 2023.