With the rise in COVID-19 cases, the interruption in dental services became inevitable. In view of the scarcity of personal protection equipment (PPE) for health professionals and the high risk of contamination, several Brazilian cities have chosen to treat only the most urgent cases within the public health system. In places where services are being resumed, the challenges of adapting to the new reality demands changes to routine procedures. Such is the case with the high-speed handpiece, popularly known as the “dental drill.” Widely used in the treatment of dental caries, or tooth decay, the tool now presents a potential risk factor for public health. This is because it produces aerosols, microscopic particles suspended in the air, increasing the exposure of patients and dentists to the Sars-CoV-2 virus, which is transmitted mainly through aerosolized saliva droplets. Experts are unanimous in stating that the health emergency brought about by the pandemic has placed a long-standing issue back at the center of the debate: the gap between scientific advances in the dental field and the treatments being offered to the general population.
“We need to make a greater effort to cultivate the relationship between the knowledge generated in academia and the dental care offered in the public health system,” says Marisa Sugaya, Oral Health Coordinator for the municipality of Suzano, in the Metropolitan Region of São Paulo. Over recent years, the municipality has established collaborations with higher education and research institutions in order to gain faster access to scientific information capable of supporting new oral health policies and procedures. In partnership with the University of Mogi das Cruzes and the University of São Paulo School of Dentistry (FO-USP), the city health system adopted a minimally invasive technique called Atraumatic Restorative Treatment (ART). “The initial goal, before the pandemic, was to expand the treatment of tooth decay in municipal schools,” Sugaya says.
– The effects of COVID-19
– Potential treatment
– The uncertainty of herd immunity
– Scientific philanthropy boost
The arrival of the pandemic reinforced the need to promote noninvasive procedures in oral healthcare services. On June 24, the Ministry of Health published an ordinance including ART on the authorized procedures list of Brazil’s Unified Health System (SUS). The method (see inset) is based on treating cavities and restoring teeth using hand tools, which do not need electricity to function. “The approach is simple and inexpensive, allowing dental problems to be solved with the same efficiency as with drills, but without anesthesia or the dental chair,” explains Fernanda Campos de Almeida Carrer. She is coordinator of the Center for Evidence in Oral Health (NEv), created in 2018, a collaborative effort of FO-USP and the World Health Organization (WHO).
Carrer says the technique isn’t new from a scientific point of view, but its application has never been well accepted in dentist’s offices. “There’s a stigma associated with ART, because the method was developed in the 1980s to treat patients in rural areas or poorer regions.” The fact that dental education programs prioritize the use of cutting-edge technologies also contributed to underestimating ART treatment, in her estimation. Its wider use could create conditions for resuming elective services that have been suspended during recent months. Since the beginning of the pandemic, the number of dental consultations conducted through SUS has dropped 80% nationwide, according to a survey conducted by the Federal University of Pelotas (UFPEL).
However, the dialogue between universities and professionals working in public health clinics shouldn’t be limited to the search for solutions only in emergencies, like the current situation, argues Vinício Felipe Brasil Rocha, a professor at José do Rosário Vellano University (UNIFENAS) and a dentist at the Dental Specialty Center of Varginha, in Minas Gerais. “Solid collaborations with research groups give managers and health professionals access to epidemiological data and new technologies capable of improving the quality and efficiency of dental treatments,” he says. Varginha was one of the first cities in the country to implement public policy based on scientific evidence in the dental field, with support from the FO-USP evidence center. Over the past two years, the partnership has made it possible to introduce health education measures facilitated by information technology, which are changing techniques and practices across various sectors of medicine and dentistry. “We also simplified the production of dental prostheses, saving time in the office, reducing costs, and increasing people’s access to this type of basic rehabilitation treatment.”
“Researchers need to be more involved in the translation of scientific knowledge into public policy proposals,” observes Marisa Sugaya
Convincing public administrators of the importance of listening more closely to scientists is crucial, Sugaya believes. There are similar gaps on the university side: “Researchers need to be more involved in the translation of scientific knowledge into public policy proposals,” she observes. The problem is that in many cases dental research is not focused on the specific needs of SUS. Although Brazilian legislation has included dental treatment as an element of primary care within the public system, the majority of dentists work in the private healthcare system.
Of the nearly 340,000 dentists working in Brazil, only 60,000 are linked to SUS. Furthermore, approximately 80% of dentistry programs are at private institutions. Because education is mostly directed toward the private dental market, the better part of research is aimed at solving problems specific to this sector. “It happens that the demands of private-sector dentistry are distinct from the needs of the majority of the population,” says Roger Keller Celeste, from the Department of Preventive and Social Dentistry at the Federal University of Rio Grande do Sul (UFRGS).
Celeste observes that the market is continually investing in cosmetic dentistry research, which has the potential to generate new products and services that add value to procedures such as implants and tooth whitening. Meanwhile, demand is still growing for research that aids in understanding the epidemiological profile of oral diseases, which today affect more than 3.5 billion people worldwide. “Tooth decay is the most prevalent all diseases, especially in low- and middle-income countries,” explains Keller, who participated in a series of international studies on oral health published in The Lancet in 2019.
The study draws attention to the need for more dental research that will speak to social and economic factors that affect the nation’s health. “Worldwide, oral health care and approaches to disease prevention still mostly operate in ways that aren’t integrated with public policies on issues like fluoridated water, dietary standards, and social inequality,” Keller says. He cites as an example the impact of sugar on the incidence of cavities. Despite advances such as increasing fluoridation in public water supplies and the amount of fluoride in toothpastes, treatment of tooth decay also requires efforts to combat excessive sugar consumption, which is the primary cause of cavities, according to the researcher. “Tooth decay is multifactorial, and has a marked interaction with cultural, behavioral, and physiological factors.” In his assessment, dental research needs to be more engaged with multidisciplinary projects dedicated to investigating social determinants that impact oral health in the populace.
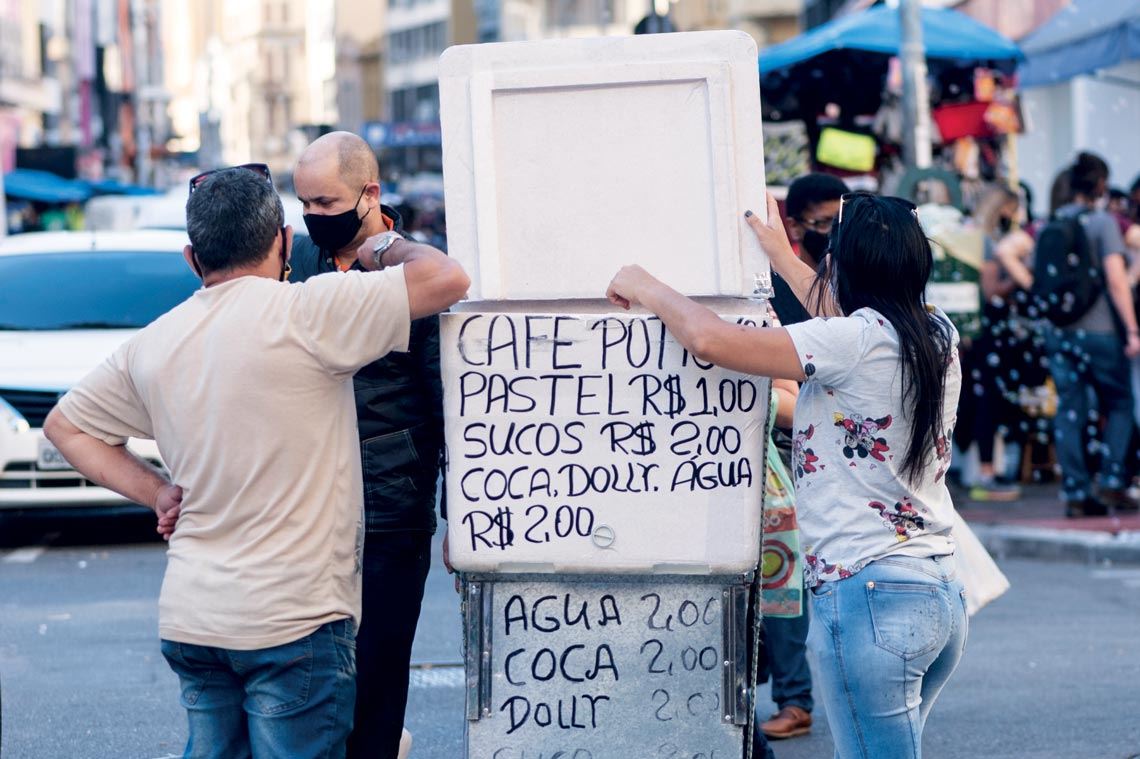
Léo Ramos Chaves
Street food: dietary standards, access to fluoridated water, and social inequality impact oral healthLéo Ramos ChavesFor example, lower per capita household income and less education influences people’s perception of their own oral health. This was shown in research published in 2019 by researchers from the Brazilian Institute of Geography and Statistics (IBGE), the University of Porto, in Portugal, and USP. Analyzing data from the 2013 National Health Survey, the authors suggest that understanding socioeconomic position indicators could contribute to improving the direction of public oral health policy for vulnerable social groups.
Another study published last year by researchers from São Paulo State University School of Dentistry (UNESP), Araçatuba campus, suggests that research in public health is still the minority in dentistry. They analyzed 3,008 papers presented at the 35th Annual Meeting of the Brazilian Society of Dental Research (SBPQO) held in 2018 and found that only 92 abstracts dealt with public projects and actions in oral health. Of this total, 46% dealt with promoting health, 27% with epidemiology, 17% with health education and 10% with oral health care. The researchers also observed that of the total number of studies analyzed, 63% were from the Southeast region, 67% from public institutions, and only 38% were financed by funding agencies, mainly by FAPESP, by the Federal Agency for Support and Evaluation of Graduate Education (CAPES), and the National Council for Scientific and Technological Development (CNPq).
In wealthy nations with universal healthcare, such as England, Canada, and Sweden, it was observed that an omission of dental care in the public system directly interferes with the types of research developed at universities. In the British model, for example, university dental hospitals attend to public-system patients, but treatment is generally restricted to highly complex services. Primary care is provided by private clinics, which may or may not be accredited with the public healthcare system. “The government has adopted a quota system, in which dentists in the private system are paid according to the type of procedure performed,” explains Mario Vettore, from the Department of Social and Preventive Dentistry at the Federal University of Minas Gerais (UFMG).
“The problem is that basic and preventive services are the lowest paid. Therefore, dentists are encouraged—even if indirectly—to opt more for interventive strategies such as tooth reconstruction, than for health-promoting actions,” says Vettore, who taught for six years in the dentistry program at the University of Sheffield, England. Consequently, he notes, the country’s research is dedicated more to developing products, such as dental instruments, and new materials, such as porcelain veneers, used in aesthetic treatments.
It may be said that Brazil occupies an intermediate position between countries that invest highly in dental-market research, and those that invest the least in this billion-dollar sector. “The fact that the National Healthcare Policy included dental treatment as an element of primary care contributed to SUS requirements being included, albeit in a limited way, in postgraduate programs, especially those focused on public health,” says Paulo Frazão, from the USP School of Public Health.

Irineu Junior
Dental treatment in Suzano: the municipality established collaborations with research institutions to gain faster access to scientific informationIrineu JuniorHe highlights the role of research dedicated to investigating how dentists are distributed across Brazil. Most are still concentrated in the more developed cities. Considered one of the most in-depth studies on the subject, Perfil atual e tendência do cirurgião-dentista brasileiro (The current profile and trends of Brazilian dental surgeons) was published in 2010 and pointed out that, at that time, Brazil had more dentists than any other country, accounting for 19% of the total number of practitioners in the world. Despite this, 57% were found in only three states: São Paulo, Minas Gerais, and Rio de Janeiro. “These professionals end up settling in regions where they will have better chances of financial success by providing services in private clinics and offices,” Frazão says.
Fernanda Tricoli, coordinator of Oral Health at the São Paulo State Department of Health, believes that the situation has not changed much over the last decade. “Dentists are usually trained to work in private practice, which ends up keeping them isolated from the larger problems related to oral health in the population where they work,” says Tricoli. She points out, however, that in 2004 the creation of the national program Brasil Sorridente [Smiling Brazil] fostered improvement by structuring a network linked with SUS, whose goal was to expand dental care to the country’s most socioeconomically vulnerable areas. “This policy created space for partnerships between SUS and the universities, providing internships so that dental students can gain experience in the public health system and with other local realities.”
Still, says Tricoli, the coverage rate of dental treatment by SUS is significantly low in Brazil. In the state of São Paulo, she reports, only 34% of the population is able to gain access. “Due to SUS underfunding, the public system ends up being more restricted to preventive actions at the local Health Clinics,” she observes. “The system even offers more complex procedures, such as orthognathic surgery to correct jaw deformities, but in low quantities, due to the lack of resources to hire specialized professionals and incorporate modern technologies.” USP’s Paulo Frazão points out that the percentage of dentists working in public dental service reaches 51% in other low-income countries, adding “In Brazil, however, the rate is only 30% to 35%.”
For this reason, Fernanda Carrer, at USP, argues that technological research not only benefits the market, but also SUS. This is because products and services initially aimed at serving a restricted segment of the population—those who can afford expensive treatments—may eventually be incorporated by SUS, if there is a positive cost-benefit result. “Dental implants, for example, were already quite popular with the elite class, but have become popular generally,” says Carrer, also citing the example of low-power lasers—an anti-inflammatory therapy—used to treat oral lesions such as herpes and the side effects of cancer treatments. “This was once very expensive equipment, but today it can be found in public dentist’s offices at Dental Specialties Centers in São Paulo,” she says.
Developed in the early 1980s by professors at the University of Groningen, in the Netherlands, Atraumatic Restorative Treatment (ART) was initially designed to expand dental care to vulnerable communities without electricity. Unlike more invasive procedures to treat tooth decay, ART drops the use of a high-speed handpiece—the “dental drill”—and can be performed away from dental offices, in places such as schools and settlements. The technique consists of removing damaged tissue from the patient’s tooth using only hand instruments such as dental tweezers, spatulas, and spoons. Subsequently, the cavity is filled with an adhesive material, a high-viscosity glass-ionomer cement, which is biocompatible and releases fluoride.
The technique’s safety and efficiency have been proven in scientific studies published during recent decades, explained Elizabeth de Souza Rocha, a researcher at the USP School of Dentistry, in a live presentation hosted by the Ibero-American Observatory of Public Policies in Oral Health. “Over time, it was realized that ART has numerous advantages,” Rocha says. One of the main benefits is the decrease in the use of anesthesia and cutting-edge technologies, which means less complex facilities are required, compared to other procedures. In addition, there is evidence that ART reduces pain during treatment, as well as the anxiety that many patients experience when going to the dentist’s office and hearing the whine of a dental drill.
The first studies to test the efficiency of ART in the field were conducted during the early 1990s in Tanzania, Thailand, and Zimbabwe. The research, led by Jo Frenken of the Netherlands, showed that the technique was not only able to remove cavities in a minimally invasive way, but also contributed to the implementation of oral health promotion programs. In 1994, the World Health Organization (WHO) recognized the importance of the procedure in combating tooth decay, especially in poorer countries. ART began to be used in Brazil, especially for treating schoolchildren, but only sporadically in some municipalities, including São Paulo. In 2002, the WHO Collaborating Center in Nijmegen, the Netherlands, published the Basic Package of Oral Care, a guide with recommendations for decision makers in the public health field. “The document is still quite current,” Rocha points out. “It defines three pillars for dental care: managing emergencies, such as pain and trauma, promoting the use of fluoride toothpaste, and treating cavities using the ART technique.”
Although it has been improved in recent decades, the method does not completely replace the use of the handpiece, Rocha said. ART is not indicated for treating deep lesions, in which the dental pulp is compromised or there are gum polyps, for example. “It is therefore essential to make an adequate diagnosis, assessing the severity of the lesion, and whether a more complex or less invasive treatment is required.”
Scientific articles
SOUSA, J. L. et al. Posição socioeconômica e autoavaliação da saúde bucal no Brasil: Resultados da Pesquisa Nacional de Saúde. Cad. Saúde Pública. Online. Vol. 35, no. 6. May 2019.
GONÇALVES, A. N. et al. Brazilian articles in top-tier dental journals and influence of international collaboration on citation rates. Brazilian Dental Journal. Vol. 30, no. 4, pp. 307–16. July 2019.
BARBOSA, L. C. et al. Overview of the Brazilian odontological studies presented at a scientific meeting – SBPqO. Revista de Odontologia da Unesp. Vol. 48 2019.
PERES, M. A. et al. Oral diseases: A global public health challenge. The Lancet. July 2019.


