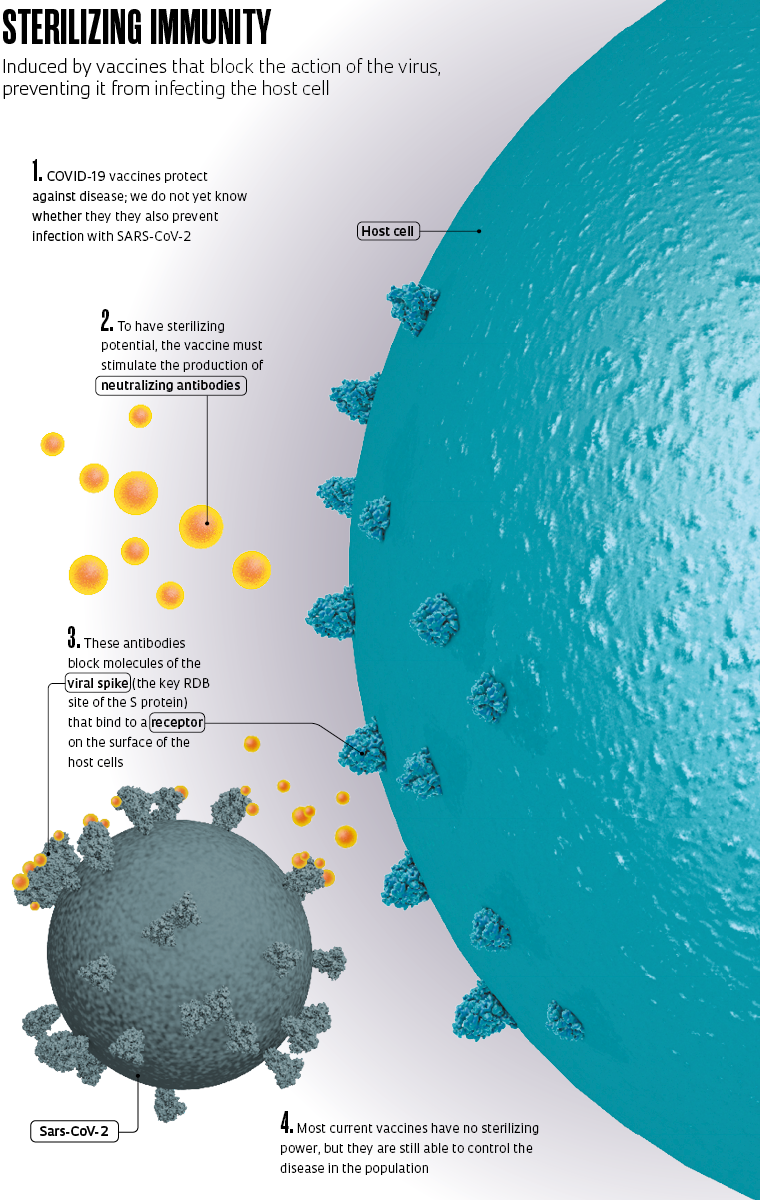
Immunization against COVID-19, the disease caused by the novel coronavirus, is progressing worldwide, bringing us closer to overcoming the current health crisis. As the process advances, we will learn more about the effect of the approved vaccines. One aspect that will become more clear over time is whether as well as protecting people from the diseease, they are also able to prevent infection by SARS-CoV-2 virus itself. Clinical studies on the vaccines in use show that they are effective at inhibiting the disease, reducing symptoms, and preventing severe outcomes, but it is not yet known whether they can also prevent the virus from invading human cells and starting the replication process. Vaccines that prevent both disease and infection induce what doctors call sterilizing immunity.
There is a subtle but important difference between stopping the infection, and consequently the disease, and protecting only against the disease. Vaccines that prevent the onset of COVID-19 do not necessarily prevent immunized people from being infected and transmitting the novel coronavirus, even if they present no symptoms and feel fine. Those that totally block the infection, providing sterilizing immunity, however, nullify the virus and interrupt the chain of contagion.
British virologist Sarah Caddy, a clinical researcher at the Cambridge Institute of Therapeutic Immunology and Infectious Disease (CITIID) at the University of Cambridge, UK, says the ideal scenario would be that all vaccines prevent infection by the pathogen, but in practice, this is not the case. Most existing vaccines only prevent onset of the disease. This is the case, for example, with the vaccines for influenza, hepatitis, measles, tuberculosis, and rotavirus.
– Combat strategy
– Obstacle course
– Breathless emerging economies
– Eurico Arruda: Admirer of viruses
“Even without blocking infection,” Caddy told Pesquisa FAPESP, “it is possible to reduce transmission and stop the COVID-19 pandemic.” This is because a vaccinated person, if infected with the novel coronavirus, will have a lower viral load than someone who has not been immunized, catches the virus, and shows symptoms. Studies indicate that asymptomatic infected people also have a lower viral load. Vaccines thus help to reduce the virus’s circulation rate, explains the expert. “Even without sterilizing immunity, a vaccine can control the disease in the population.”
According to infectious disease specialist Raquel Stucchi of the School of Medical Sciences (FCM) at the University of Campinas (UNICAMP), the current COVID-19 vaccines can help us achieve herd immunity, where the spread of the virus is contained because there are so few people susceptible to contracting it. “It is possible to achieve herd immunity against the novel coronavirus even without having complete control over its transmission. To do so, we need to vaccinate a larger contingent of the population,” says Stucchi. “Of course, it would be a great help if we had a vaccine that also prevents transmission, but it is not essential. Today we have several vaccines in our portfolio that despite not conferring sterilizing immunity, are capable of controling the disease for which they were developed.”