In an effort to accelerate the collection and sharing of data on how to treat people infected with the new coronavirus (SARS-CoV-2), which causes COVID-19, the World Health Organization (WHO) began a global study at the end of March, involving patients from multiple countries, to test the drugs that have shown the most promise against the disease to date. Before being launched on the consumer market, new drugs or vaccines must be approved by official regulatory agencies, which require them to pass several tests that prove their safety and efficacy in humans (view infographic). One of the strategies being used to accelerate this process is to evaluate the effects of medications that have already been clinically approved and used against other diseases.
It is estimated that up to 70 drugs—some commercially available and others still in testing—have some effect on the new coronavirus. One is hydroxychloroquine, derived from chloroquine and originally used to treat malaria. The drug has been widely debated since the publication of apparently promising—albeit preliminary—results of human trials carried out in France and China. These studies, carried out urgently in the midst of the pandemic, may have lacked the usual scientific rigor, but they grew in prominence after American President Donald Trump claimed that the US Food and Drug Administration (FDA) had approved the use of hydroxychloroquine for COVID-19 patients. In Brazil, President Jair Bolsonaro, despite the lack of evidence, also promoted the drug as a treatment for the disease.
Recent studies, however, have yielded less encouraging results. There are indications that the use of hydroxychloroquine in individuals with COVID-19 may trigger serious adverse reactions, especially when administered alongside other medications in people with preexisting kidney or heart disease. The evidence prompted the FDA to issue a statement on April 24 expressing concern about the use of the drug in COVID-19 patients. The agency recommended that it be used only in clinical trials or hospitals, where patients are closely monitored by medical staff.
The main suspicion is that hydroxychloroquine increases the risk of complications such as cardiac arrhythmia—heart rate changes that can cause problems ranging from malaise to cardiac arrest. In Brazil, a study carried out in Manaus by researchers from various institutions to evaluate the use of two different dosages of the drug in people with COVID-19 had to be stopped after 11 participants died. Some of them had received higher doses of the drug, which may have triggered fatal heart complications. Another study published in April on the medRxiv repository assessed the use of hydroxychloroquine in 368 men with COVID-19, of whom 97 were given hydroxychloroquine, 113 hydroxychloroquine and azithromycin together, and 158 another treatment. The results showed that 27% of patients treated with hydroxychloroquine died, as did 22% of those who received the combination therapy. The mortality rate of the third group was 11.4%.

Reuters / Fotoarena
Researchers in a lab evaluate the effects of hydroxychloroquine on samples of the new coronavirus
Reuters / FotoarenaHydroxychloroquine is a less toxic version of chloroquine, a medication developed in 1934 and used to prevent and treat malaria. Interest in the drug was sparked by a letter published in the journal BioScience Trends by Chinese researchers in March, suggesting that the drug may be capable of inhibiting the proliferation of SARS-CoV-2 in infected people. “The problem is that the authors did not disclose the data behind their conclusions, making it impossible to reproduce the results or even to assess whether they make any sense,” says doctor Marcelo Urbano Ferreira, from the Institute of Biomedical Sciences at the University of São Paulo (ICB-USP).
Expectations about the drug were later reinforced by a controversial study of 36 COVID-19 patients published in the International Journal of Antimicrobial Agents, in which French researchers claimed to have obtained promising results when using it to treat individuals with the disease. The study examined the effectiveness of hydroxychloroquine when administered alone and in conjunction with azithromycin in patients admitted to a hospital in Marseille, southern France. According to pharmacologist Gustavo Batista de Menezes, from the Institute of Biological Sciences at the Federal University of Minas Gerais (UFMG), the French study has some hidden flaws that make its results less compelling. “The research fails in practically all the basic requirements of a good clinical trial,” he says.
Despite the controversy, some hospitals around the world have experimentally incorporated hydroxychloroquine into their COVID-19 treatment plan. On March 26, Brazilian health insurance provider Prevent Senior started tests of hydroxychloroquine and azithromycin in 412 COVID-19 patients at one of its hospitals in the city of São Paulo. Preliminary results, released on April 17, suggested that the strategy had reduced the number of hospitalizations. The problem is that the company started the trial before receiving authorization from the National Research Ethics Commission (CONEP) and conducted no laboratory tests to confirm that the patients had actually been infected with SARS-CoV-2. As a result, CONEP suspended the study.
According to Marcelo Ferreira, the controversies surrounding hydroxychloroquine reinforce the need for more robust studies to assess whether the drug is safe and effective against Covid-19. “These studies will also help to identify potential side effects associated with its administration in people with the disease,” says biologist Cláudio Marinho, from ICB-USP.
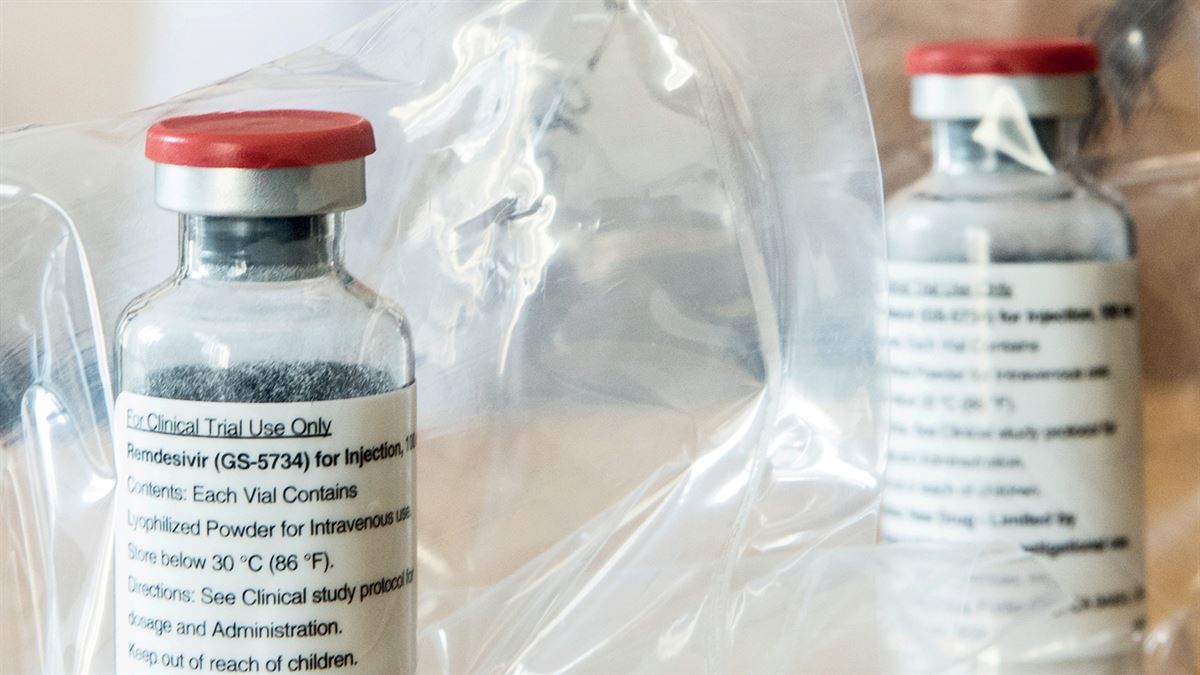
Antivirals and monoclonal antibodies
Although the controversial use of hydroxychloroquine against COVID-19 has dominated the public debate, other compounds, especially antivirals, are also being tested against the disease. One example is remdesivir, developed by North American company Gilead Sciences to treat Ebola. In March, the company announced the start of clinical trials to evaluate its efficacy and safety in almost 1,000 people. As well as the WHO and Gilead Sciences, researchers from public institutions are also studying the drug’s potential. On April 29, scientists from the National Institute of Allergy and Infectious Diseases, one of the USA’s National Institutes of Health (NIH), published encouraging preliminary results of the use of remdesivir. In the study, of 1,063 volunteers hospitalized with COVID-19, those treated with the compound spent less time in hospital than those who received a placebo.
Scientists are also looking at lopinavir and ritonavir, two antiretrovirals used together against the HIV virus, as well as anti-inflammatory corticosteroid dexamethasone, which can cause multiple side effects and should not be taken without medical advice. In Brazil, doctors and researchers at Coalizão Covid Brasil are preparing to evaluate these drugs in clinical studies involving 290 people over the coming months, with results expected in August. The coalition was established in March by the Albert Einstein Hospital, Hospital do Coração (HCOR), and Hospital Sírio-Libanês, in addition to the Brazilian Research in Intensive Care Network (BRICNET).
The researchers are also investing in treatments capable of reducing the high concentration of inflammatory cytokines seen in the more serious COVID-19 cases. It is not uncommon for patients with these conditions to have elevated levels of a protein called interleukin-6 (IL-6) in their blood, the accumulation of which can lead to further complications and death. Studies suggest that Actemra (tocilizumab), a monoclonal antibody produced by pharmaceutical company Roche, may act as an inhibitor of IL-6. The drug, currently used to treat rheumatoid arthritis, is already being tested on people with COVID-19 in China. In March, the FDA in the USA granted Roche authorization to start clinical trials of Actemra in 300 COVID-19 patients hospitalized with pneumonia. Pharmaceutical companies Sanofi and Regeneron are also planning to test Kevzara (sarilumab), another IL-6 inhibitor, on critically ill patients.
Plasma
Hospitals and universities around the world are investigating the use of plasma from people who have recovered from COVID-19 in individuals still infected with the disease. Plasma is the liquid part of the blood and constitutes about 60% of its total content. It is being evaluated as a potential means of providing the antibodies to people whose bodies do not yet produce them at levels capable of protecting them from the disease. Although it is not a risk-free process, it is estimated that plasma transfusions can decrease viral load and help to alleviate symptoms and improve clinical outcomes.
The strategy has been used several times throughout history during outbreaks of other respiratory infections, including recent epidemics caused by other coronaviruses, such as Severe Acute Respiratory Syndrome (SARS) in 2003 and Middle East Respiratory Syndrome (MERS) in 2012. In Brazil, the Hematology and Hemotherapy Center at the University of Campinas (UNICAMP) will soon begin collecting plasma from people who have recovered from COVID-19 to treat individuals with the disease at the School of Medical Sciences (FCM) at its teaching hospital, as well as at other hospitals in the region. In early April, a consortium involving Albert Einstein Hospital, Hospital Sírio-Libanês, and USP’s School of Medicine was given authorization to begin testing plasma on people infected with the new coronavirus in critical condition. The Ribeirão Preto Blood Center has also started collecting plasma from recovered patients to treat critically ill individuals at the USP Ribeirão Preto Medical School’s teaching hospital.
“All of the evidence suggests that it will be quite some time before we have a safe and effective treatment against COVID-19,” comments Menezes. “This is because in order to properly test new strategies, we first carry out good clinical trials, which require time and human and financial resources.”
Vaccines being tested on humans Six of more than 70 formulations in development have reached the initial phases of clinical trialsAt least 76 COVID-19 vaccine candidates have emerged since the pandemic began, according to data from the WHO. However, only six have so far progressed to the human trials phase.
The most recent to reach this stage was developed by American pharmaceutical Pfizer in partnership with German biotechnology company BioNTech. On April 22, the Paul-Ehrlich Institute—Germany’s medical regulatory agency—authorized the start of phase 1 and 2 trials.
The vaccine is based on the use of synthetic SARS-CoV-2 messenger RNA (mRNA) molecules that contain the chemical recipe for producing the S-protein, used by the virus to enter human cells. The idea is that these synthetic molecules stimulate an immune response inside the cells that then prepares the body to fight the real virus. The vaccine will be tested on about 200 healthy people aged 18 to 55 over the next few months. The companies behind the vaccine are also awaiting FDA authorization to begin clinical trials in the USA.
The first vaccine candidate for the new coronavirus to reach phase 2 of clinical trials was created by Chinese company CanSino in partnership with the Beijing Institute of Biotechnology. The formulation uses a genetically modified version of adenovirus type 5 to carry synthetic SARS-CoV-2 mRNA molecules. This strategy was also used by researchers at the University of Oxford, UK, to develop their COVID-19 vaccine, which has been tested on 1,110 volunteers since late April.
Since March 16, a team from Kaiser Permanente, a health research institute in Seattle, USA, has been working with biotechnology company Moderna on phase 1 clinical trials involving 45 participants for another vaccine candidate based on SARS-Cov-2 mRNA. Another candidate in phase 1 trials was developed by Chinese biopharmaceutical company Sinovac Biotech. The vaccine, which is based on a chemically inactivated version of SARS-CoV-2, was the first to produce immunity in animals and is now being tested on 144 volunteers from the Jiangsu province in China.
The sixth formulation in human trials is being developed by American company Inovio Pharmaceuticals. The vaccine, which uses a strategy similar to the mRNA approach, began phase 1 testing on humans in early April.
In Brazil, the quest for a vaccine is still in the preclinical studies phase, currently being tested on animals. Researchers from the Oswaldo Cruz Foundation (FIOCRUZ) in Minas Gerais are trying to modify the influenza A (H1N1) virus, which causes the flu, to carry the genetic material of SARS-CoV-2 and induce an immune response in the recipient. A group from the Immunology Laboratory at FM-USP’s Heart Institute, on the other hand, has opted for a different approach to try to activate the immune system against SARS-CoV-2. They intend to combine virus-like particles (VLPs), normally recognized as an invading agent by the body, with antigens produced by the new coronavirus, to see if such a strategy can promote the production of antibodies against SARS-CoV-2.
Republish